This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing the text to give it early visibility.
Virology
Shang J, Han N, Chen Z, et al. Compositional diversity and evolutionary pattern of coronavirus accessory proteins. Briefings in Bioinformatics, October 30, 2020, bbaa262. Full-text: https://doi.org/10.1093/bib/bbaa262
Accessory proteins play important roles in the interaction between coronaviruses and their hosts. The authors developed a standardized genome annotation tool for coronavirus (CoroAnnoter) by combining open reading frame prediction, transcription regulatory sequence recognition and homologous alignment. This tool builds a comprehensive profile for coronavirus accessory proteins covering their composition, classification, evolutionary pattern and host interaction.
Transmission
Wang Y, Xu G, Huang YW. Modeling the load of SARS-CoV-2 virus in human expelled particles during coughing and speaking. PLoS One. 2020 Oct 30;15(10):e0241539. PubMed: https://pubmed.gov/33125421 . Full-text: https://doi.org/10.1371/journal.pone.0241539
The authors investigated the dependence of airborne viral load on the size distributions of the human expelled particles from coughing and speaking. Of note, differentiating “aerosols” and “droplets” using a specific size, e.g., 5 μm, did not reflect the actual evolution of virus-containing particles over time and space, because a large number of particles above 5 μm remained airborne after an extended period of time. Simulation showed that after ten seconds of a cough, although most evaporated particles are larger than 5 μm, 59.5% of the original virus-containing particles were still able to remain airborne. Simulation also showed that wearing a mask can effectively reduce the spread of the viruses. The results challenge the false dichotomy of using aerosols and droplets to separate the modes of disease transmission.
Vaccine
Kahn JP, Henry LM, Mastroianni C, et al. Opinion: For now, it’s unethical to use human challenge studies for SARS-CoV-2 vaccine development. PNAS October 29, 2020. Full-text: https://doi.org/10.1073/pnas.2021189117
Important comment: see title. According to the authors, human challenge studies (HCS) to address SARS-CoV-2 face unacceptable ethics challenges, and, further, undertaking them would do a disservice to the public by undermining already strained confidence in the vaccine development process. Ultimately, the social value of these HCS (in terms of deaths averted) hinges on the premise that people at greatest risk of COVID-19-related mortality will receive a safe and efficacious vaccine sooner than they would without HCS. Read why this will be probably not the case and why HCS would do more harm than good.
Diagnostics
Ward H, Cooke G, Atchison C, et al. Declining prevalence of antibody positivity to SARS-CoV-2: a community study of 365 000 adults. [Preprint] 2020. Full-text: https://www.imperial.ac.uk/media/imperial-college/institute-of-global-health-innovation/MEDRXIV-2020-219725v1-Elliott.pdfdoi:10.1101/2020.10.26.20219725.
Not yet peer reviewed, but important data. Results from the large, nation-wide REACT (real time assessment of community transmission) antibody study which was led by Imperial College London, show that the national antibody prevalence in the UK was 6% around 12 weeks after the epidemic’s April peak. Since then, the rates had fallen to 4.4% 24 weeks after the peak. These data suggest that antibodies induced by natural infection may be short lived, as is the case for other seasonal coronaviruses.
Henss L, Scholz T, von Rhein C, et al. Analysis of humoral immune responses in SARS-CoV-2 infected patients. J Infect Dis. 2020 Oct 31:jiaa680. PubMed: https://pubmed.gov/33128369 . Full-text: https://doi.org/10.1093/infdis/jiaa680
Do previous coronavirus infections protect from severe courses? Lisa Henss and colleagues from Frankfurt University analyzed the humoral immune response of a cohort of 143 COVID-19 patients, using ELISA and neutralization assays. Disease severity correlated with the amount of SARS-CoV-2 specific IgG and IgA and the neutralization activity of the antibodies. Neutralizing titers of patients with mild disease were very low and higher titers were only detected in severe cases. Of note, compared to patients with mild-moderate disease, patients with severe disease had only weakly neutralizing antibodies against coronavirus-NL63. Although the numbers of severe cases were low, it remains tempting to speculate that preexisting immunity to NL63 or other common cold coronaviruses might reduce the risk of severe disease.
Clinical
Hoffmann C, Wolf E. The Low Case Fatality Rate of COVID-19 in Hong Kong Could Be Deceptive. Clin Infect Dis. 2020 Oct 29:ciaa1676. PubMed: https://pubmed.gov/33119056 . Full-text: https://doi.org/10.1093/cid/ciaa1676
Last Monday, we published data from the 20 most affected European countries and the USA and Canada, showing that during the first wave of the pandemic, the variance of crude CFR of COVID-19 was predominantly (80-96%) determined by the proportion of older individuals who are diagnosed with SARS-CoV-2 (Hoffmann 2020).
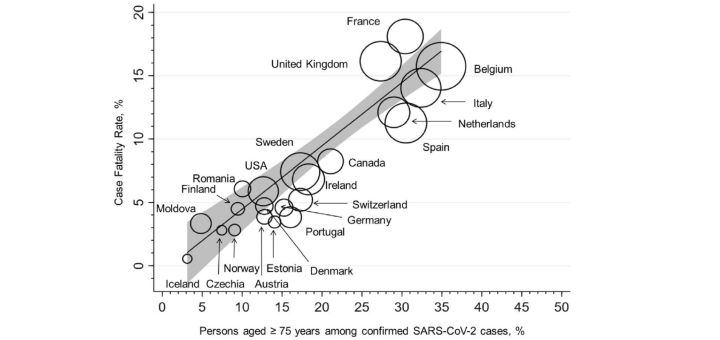
Figure 1. Association between case fatality rate (CFR) and the proportion of persons over 75 years of age among all confirmed SARS-CoV-2 cases (R2 = 0.8034, p < 0.0001). The circle sizes reflect the countryspecific numbers of COVID- 19-associated deaths per million habitants; the linear fit prediction plot with a 95% confidence interval was estimated by weighted linear regression (weight = total number of COVID-19-associated deaths). Reproduced with permission.
Here we show that our model applies to other countries. In Hong Kong, for example, a very low CFR of only 0.4% has been reported during the first weeks (Lui GC 2000). In contrast to the authors, we believe that this was mainly due to the low number of older persons among the confirmed SARS-CoV-2 cases. We also show that the overall CFR in Hong Kong has increased since then, paralleling the increasing proportion of older persons among confirmed cases. Thanks to the incredible speed of Clinical Infectious Diseases’ publishing policies (contrasting many other journals), the authors from Hong Kong have been already able to respond (in some points they agree, in other points they don’t). Please read the discussion (Lui GC 2000).
Why is this important? In many countries facing a low CFR during the first wave, there is a widespread feeling that this was mainly due to a good health care system such as ICU or testing capacities. We believe that this perception can be deceptive and that the picture in these countries will change immediately when more elderly people are infected.
Hoffmann C, Wolf E. Older age groups and country-specific case fatality rates of COVID-19 in Europe, USA and Canada. Infection. 2020 Oct 24:1-6. PubMed: https://pubmed.gov/33098532 . Full-text: https://doi.org/10.1007/s15010-020-01538-w
Lui GC, Yip TC, Wong VW, et al. Significantly Lower Case-fatality Ratio of Coronavirus Disease 2019 (COVID-19) than Severe Acute Respiratory Syndrome (SARS) in Hong Kong-A Territory-Wide Cohort Study. Clin Infect Dis. 2020 Oct 1:ciaa1187. PubMed: https://pubmed.gov/33005933. Full-text: https://doi.org/10.1093/cid/ciaa1187
Lui CG, Yip TC, Hui D, et al. Reply to Hoffmann and Wolf. Clinical Infectious Diseases, October 29, ciaa1678, https://doi.org/10.1093/cid/ciaa1678. Download PDF.
Lim ZJ, Subramaniam A, Reddy MP, et al. Case Fatality Rates for COVID-19 Patients Requiring Invasive Mechanical Ventilation: A Meta-analysis. Am J Respir Crit Care Med. 2020 Oct 29. PubMed: https://pubmed.gov/33119402 . Full-text: https://doi.org/10.1164/rccm.202006-2405OC
Definitive hospital outcome on 13,120 patients receiving invasive mechanical ventilation. Among studies where age-stratified CFR was available, pooled CFR estimates ranged from 47.9% (95% CI 46.4-49.4%) in younger patients (age ≤40) to 84.4% (95% CI 83.3-85.4) in older patients (age >80). CFR was also higher in early COVID-19 epicenters.
Prieto-Alhambra D, Balló E, Mora N, et al. Filling the gaps in the characterization of the clinical management of COVID-19: 30-day hospital admission and fatality rates in a cohort of 118 150 cases diagnosed in outpatient settings in Spain. International Journal of Epidemiology, October 29, 2020, dyaa190. Full-text: https://doi.org/10.1093/ije/dyaa190
Filling the missing link in the natural history of COVID-19, from first (usually milder) symptoms to hospitalization and/or death, the authors characterized a huge number of COVID-19 patients at the time at which they were diagnosed in outpatient settings and estimated 30-day hospital admission and fatality rates. In the month after diagnosis, 14.8% (14.6–15.0) were hospitalized, with a greater proportion of men and older people, peaking at age 75–84 years. Thirty-day fatality was 3.5%, higher in men, increasing with age and highest in those residing in nursing homes (24.5%).
Kim T, Roslin M, Wang JJ, et al. Body Mass Index as a Risk Factor for Clinical Outcomes in Patients Hospitalized with COVID-19 in New York. Obesity (Silver Spring). 2020 Oct 31. PubMed: https://pubmed.gov/33128848 . Full-text: https://doi.org/10.1002/oby.23076
Risk factor obesity. In total, 10,861 COVID‐19 patients admitted to the Northwell Health system hospitals during March and April, were classified according to their BMI: underweight (2%), normal (only 23%!), overweight (38%), obesity class I (22%), II (9%), and III (7%). Patients who were overweight (OR=1.27), obesity class I (OR=1.48), obesity class II (OR=1.89), and obesity class III (OR=2.31) had increased risk of requiring invasive mechanical ventilation. Overall, underweight and obesity classes II and III were statistically associated with death (OR=1.25-1.61). However, once mechanically ventilated, all patients regardless of BMI had similar odds of death.
Treatment
Chow JH, Khanna AK, Kethireddy S, et al. Aspirin Use is Associated with Decreased Mechanical Ventilation, ICU Admission, and In-Hospital Mortality in Hospitalized Patients with COVID-19. Anesth Analg. 2020 Oct 21. PubMed: https://pubmed.gov/33093359 . Full-text: https://doi.org/10.1213/ANE.0000000000005292
Aspirin may help (a little bit). In this retrospective, observational cohort study of 412 adult patients admitted with COVID-19 to multiple US hospitals between March and July, 98 (24%) received aspirin within 24 hours of admission or 7 days prior to admission. Aspirin use had a crude association with less mechanical ventilation (36% vs. 48%, p=0.03) and ICU admission (39% vs. 51%, p=0.04), but no crude association with in-hospital mortality (26% vs. 23% p=0.51). After adjusting for 8 confounding variables, aspirin use was independently associated with decreased risk of mechanical ventilation (adjusted HR 0.56, 95% CI 0.37-0.85, p=0.007), ICU admission (adjusted HR 0.57, 95% CI 0.38-0.85, p=0.005), and in-hospital mortality (adjusted HR 0.53, 95% CI 0.31-0.90, p=0.02). According to the authors, a sufficiently powered randomized controlled trial is needed.
