22 November
Worobey M. Dissecting the early COVID-19 cases in Wuhan. Science November 18, 2021. https://www.science.org/doi/10.1126/science.abm4454
Interesting perspective, providing insights on what happened on Huanan Market in December 2019. A new patient zero? More questions than answers.
Gharpure R, Sami S, Vostok J, et al. SARS-CoV-2 infections, including COVID-19 vaccine breakthrough infections, associated with large public gatherings, United States. Emerg Infect Dis November 18, 2021. https://doi.org/10.3201/eid2801.212220
A large outbreak, occurring in Provincetown, Massachusetts. During July 3–17, thousands of visitors traveled to Provincetown and participated in large, densely packed indoor and outdoor gatherings “marketed to adult male participants” (or “carnival”, see picture below). Multiple continuous events were held at venues such as restaurants, bars, and guest houses. Not the best idea: Among the 1128 cluster-associated primary and secondary cases, the authors identified 918 (81%) vaccine breakthrough cases. This investigation highlights that Delta can spread quickly through a highly vaccinated population and can be transmitted to others regardless of vaccination status. Probably the worst news during these dark days.
Talic S, Shah S, Wild H, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ November 18, 2021; 375. https://www.bmj.com/content/375/bmj-2021-068302
In this systematic review and meta-analysis, several personal protective and social measures, including handwashing (relative risk 0.47), mask wearing (0.47), and physical distancing (0.75) were associated with reductions in the incidence of COVID-19. However, owing to the heterogeneity of the studies, meta-analysis was not possible for the outcomes of quarantine and isolation, universal lockdowns, and closures of borders, schools, and workplaces.
17 November
Boon SS, Wong MC, Ng RW, et al. Seroprevalence of Unidentified SARS-CoV-2 Infection in Hong Kong During 3 Pandemic Waves. JAMA Netw Open November 15, 2021;4(11):e2132923. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2786137
Until April 2021, more than 99.5% of the general population of Hong Kong remained naive to SARS-CoV-2.
15 November
Stafford N. Covid-19: Germany’s doctors call for clear rules to “break chains of infection” as cases soar. BMJ 2021 November 12;375:n2783. https://www.bmj.com/content/375/bmj.n2783
You could call it “urgent”.
13 November
Ganslmeier M, Furceri D, Ostry JD. The impact of weather on COVID-19 pandemic. Sci Rep November 11, 2021, 22027. https://doi.org/10.1038/s41598-021-01189-3
Not new: a negative association between temperature and the spread of the virus. However, the empirical evidence of this work suggests that weather’s containment effects are largest at mealtimes, when weather has a substantial impact on the likelihood of social gatherings held indoors versus outdoors. Data also indicate that temperature has larger effects when containment measures are lifted and mobility is greater.
No good prospects these days in Europe.
5 November
Trauer JM, Lydeamore MJ, Dalton GW, et al. Understanding how Victoria, Australia gained control of its second COVID-19 wave. Nat Commun November 1, 2021, 12, 6266. https://www.nature.com/articles/s41467-021-26558-4
Face coverings had a considerably greater effect on reversing the epidemic than behavioural changes. Individual-level effect of physical distancing was 37.4% (95%CrI 7.2−56.4%) and 45.9% (95%CrI 32.9−55.6%) of face coverings.
1 November
Schulz C, Martina B, Mirolo M, et al. SARS-CoV-2–specific antibodies in domestic cats during first COVID-19 wave, Europe. Emerg Infect Dis October 25, 2021. https://doi.org/10.3201/eid2712.211252
Among > 2000 domestic cats from 4 countries during the first coronavirus disease wave in Europe, the authors found 4.4% seroprevalence using a virus neutralization test, demonstrating probable human-to-cat transmission. (Joshua claims he has no cat).

30 October
Sonabend R, Whittles LK, Imai N, et al. Non-pharmaceutical interventions, vaccination, and the SARS-CoV-2 delta variant in England: a mathematical modelling study. Lancet October 27, 2021. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)02276-5/fulltext
Main message: with the Delta variant, it might not be possible to fully lift NPIs without a third wave of hospital admissions and deaths, even if vaccination coverage is high.
26 October
Mashe T, Takawira FT, de Oliveira Martins L, et al. Genomic epidemiology and the role of international and regional travel in the SARS-CoV-2 epidemic in Zimbabwe: a retrospective study of routinely collected surveillance data. Lancet Global Health October 22, 2021. https://doi.org/10.1016/S2214-109X(21)00434-4
International and regional migration (compared to local migration) was the predominant driver of SARS-CoV-2 transmission in Zimbabwe during the early phases of the pandemic.
23 October
Lalwani P, Araujo-Castillo RV, Ganoza CA, et al. High anti-SARS-CoV-2 antibody seroconversion rates before the second wave in Manaus, Brazil, and the protective effect of social behaviour measures: results from the prospective DETECTCoV-19 cohort. Lancet Global Health November 1, 2021. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(21)00355-7/fulltext
The city of Manaus, Brazil, has seen two collapses of its health system due to the COVID-19 pandemic. Based on blood donor antibody surveillance, the cumulative proportion of the population infected was estimated to be more than 70%. This study shows that several modifiable behaviors increased the risk of seroconversion, including non-compliance with non-pharmaceutical interventions measures such as not wearing a mask during contact, relaxation of protective measures like distancing, and non-remote working.
Buss LF, Sabino EC. Intense SARS-CoV-2 transmission among affluent Manaus residents preceded the second wave of the epidemic in Brazil. Lancet Global Health, November 1, 2021. https://doi.org/10.1016/S2214-109X(21)00396-X
Lewis Buss and Ester Sabino conclude that “The results highlight heterogeneities in transmission and hint at a possible asynchronous COVID-19 peak among more affluent Manaus residents who were better able to isolate during the first wave.”
19 October
Yang B, Sullivan SG, Du Z, Tsang TK, Cowling BJ. Effectiveness of international travel controls for delaying local outbreaks of COVID-19. Emerg Infect Dis October 13, 2021. https://wwwnc.cdc.gov/eid/article/28/1/21-1944_article
Analyzing data from 165 countries the authors found that early implementation of international travel controls led to a mean delay of 5 weeks in the first epidemic peak of cases.
10 October
Arık SÖ, Shor J, Sinha R, et al. A prospective evaluation of AI-augmented epidemiology to forecast COVID-19 in the USA and Japan. npj Digit. Med. 4, 146 (2021). https://doi.org/10.1038/s41746-021-00511-7
The authors present an artificial intelligence (AI)-augmented forecast modeling framework that provided daily predictions of the expected number of confirmed COVID-19 deaths, cases, and hospitalizations over the next 4 weeks. Their simulations might also indicate what non-pharmaceutical interventions (alongside vaccinations) might be essential for faster recovery from the pandemic.
7 October
Giuliani R, Cairone C, Tavoschi L, et al. COVID-19 outbreak investigation and response in a penitentiary setting: the experience of a prison in Italy, February to April 2020. Euro Surveill. 2021 Sep;26(38). PubMed: https://pubmed.gov/34558404. Full text: https://doi.org/10.2807/1560-7917.ES.2021.26.38.2001385
In Italy, the median age of people in prison is between 50 and 55 years. The study describes an outbreak of COVID-19 in a prison situated in the city of Milan at the beginning of the Italian epidemic in late winter 2020. The attack rate (AR) was highest among custodial staff with 17.6% (94/535 including probable cases) followed by the healthcare workers with 8.8% (7/80) and the people in prison with 2.5% (22/865).
6 October
Shitrit P, Zuckerman NS, Mor O, Gottesman BS, Chowers M. Nosocomial outbreak caused by the SARS-CoV-2 Delta variant in a highly vaccinated population, Israel, July 2021. Euro Surveill. 2021 Sep;26(39). PubMed: https://pubmed.gov/34596015. Full text: https://doi.org/10.2807/1560-7917.ES.2021.26.39.2100822
The authors describe an investigation of a COVID-19 outbreak in Israel that started from one unidentified COVID-19 patient (mid-July 2021), with extensive, rapid nosocomial spread. Of the 42 cases in this outbreak, 38 were fully vaccinated with two doses of the BioNTech/Pfizer vaccine. The attack rate among exposed individuals reached 23.3% in patients and 10.3% in staff. Worryingly, “several transmissions probably occurred between two individuals both wearing surgical masks, and in one instance using full PPE, including N-95 mask, face shield, gown and gloves.”
4 October
Tonzel JL, Sokol T. COVID-19 Outbreaks at Youth Summer Camps — Louisiana, June–July 2021. MMWR Morb Mortal Wkly Rep. ePub: 1 October 2021. Full text: http://dx.doi.org/10.15585/mmwr.mm7040e2
Widespread circulation of the fairly transmissible Delta variant and underutilization of preventive measures such as vaccination, masking, and physical distancing? Not good. The authors report 28 camping outbreaks in Louisiana (US), which included a total of 321 COVID-19 cases among an estimated 2988 campers and staff members. The mean outbreak size was 11.5 cases (range = 2–59 cases). Compared with the June–July period of 2020, when only two outbreaks were identified in Louisiana, this represents a thirty-one-fold increase in confirmed camp-associated cases.
3 October
Dyson L, Hill EM, Moore S, et al. Possible future waves of SARS-CoV-2 infection generated by variants of concern with a range of characteristics. Nat Commun. 2021 Sep 30;12(1):5730. PubMed: https://pubmed.gov/34593807. Full text: https://doi.org/10.1038/s41467-021-25915-7
How will new variants shape future COVID-19 waves? As expected, the authors’ model demonstrate that a new strain with a substantial transmission advantage over resident variants, or with immune escape properties, can generate a wave of infections and hospitalizations comparable to previous waves. “Moreover, a variant that is less transmissible, but shows partial immune-escape could provoke a wave of infection that would not be revealed until control measures are further relaxed.”
29 September
Vam Loon W, Theuring S, Hommes F, et al. Prevalence of SARS-CoV-2 Infections Among Students, Teachers, and Household Members During Lockdown and Split Classes in Berlin, Germany. JAMA Netw Open. 2021;4(9):e2127168. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2784548?resultClick=1
Only a few isolated SARS-CoV-2 infections, no clusters in early 2021.
28 September
Jehn M, McCullough JM, Dale AP, et al. Association Between K–12 School Mask Policies and School-Associated COVID-19 Outbreaks — Maricopa and Pima Counties, Arizona, July–August 2021. MMWR Morb Mortal Wkly Rep September 24, 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7039e1.htm?s_cid=mm7039e1_w
Still any doubts? Please forward to all your friends, especially the mask-doubters! After adjusting for potential confounders, the odds of a school-associated COVID-19 outbreak in schools without a mask requirement were 3.5 times higher than those in schools with an early mask requirement (95% CI: 1.8–6.9).
Budzyn SE, Panaggio MJ, Parks SE, et al. Pediatric COVID-19 Cases in Counties With and Without School Mask Requirements — United States, July 1–September 4, 2021. MMWR 24 September 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7039e3.htm?s_cid=mm7039e3_w
Same idea: after controlling for co-variates, school mask requirements remain associated with lower daily case rates of pediatric COVID-19 (β = −1.31; 95% confidence interval: −1.51 to −1.11) (p < 0.001).
25 September
Giuliani R, Cairone C, Tavoschi L, et al. COVID-19 outbreak investigation and response in a penitentiary setting: the experience of a prison in Italy, February to April 2020. Euro Surveill. 2021;26(38):pii=2001385. https://doi.org/10.2807/1560-7917.ES.2021.26.38.2001385
An outbreak of COVID-19 within a prison in Italy. The infection spread not only among cellmates but also among individuals living in contiguous cells and sharing adjacent spaces. Transmission was more common between detained individuals with a shared culture or language, forming micro-clusters.
23 September
Hagan LM, McCormick DW, Lee C, et al. Outbreak of SARS-CoV-2 B.1.617.2 (Delta) Variant Infections Among Incarcerated Persons in a Federal Prison — Texas, July–August 2021. MMWR 21 September 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7038e3.htm?s_cid=mm7038e3_w
Bad news from this federal prison in Texas. During an outbreak involving the Delta variant, transmission was incredibly high among vaccinated (70%) and unvaccinated (93%) persons. Although hospitalizations, deaths, and attack rates were higher among unvaccinated than vaccinated persons, the duration of positive serial PCR test results was similar between these two groups, and infectious virus was cultured from both vaccinated and unvaccinated participants. This underscores the importance of implementing and maintaining multiple COVID-19 prevention strategies.
16 September
Young BC, Eyre DW, Kendrick S, et al. Daily testing for contacts of individuals with SARS-CoV-2 infection and attendance and SARS-CoV-2 transmission in English secondary schools and colleges: an open-label, cluster-randomised trial. Lancet September 14, 2021. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01908-5/fulltext
In this huge controlled study, supervised daily testing with lateral flow devices was non-inferior to self-isolation for close contacts to control SARS-CoV-2 transmission. However, school absence was not significantly reduced due to daily testing.
15 September
Love J, Keegan LT, Angulo FJ, et al. Continued need for non-pharmaceutical interventions after COVID-19 vaccination in long-term-care facilities. Sci Rep 11, 18093 (2021). https://doi.org/10.1038/s41598-021-97612-w
A stochastic model to simulate outbreaks in LTCF populations with differing vaccination coverage and NPI adherence to evaluate their interactive effects. Bottom line: to prevent further illness and deaths, there is a continued need for NPIs in LTCFs during vaccine rollout.
Davis EL, Lucas TCD, Borlase A, et al. Contact tracing is an imperfect tool for controlling COVID-19 transmission and relies on population adherence. Nat Commun 12, 5412 (2021). https://www.nature.com/articles/s41467-021-25531-5
Well-implemented contact tracing could provide up to a 15% reduction in R but is not currently appropriate as the sole measure of control. Reporting and adherence are the most important predictors of programme impact but tracing coverage and speed also play an important role.
14 September
Sanders JG, Spruijt P, van Dijk M, et al. Understanding a national increase in COVID-19 vaccination intention, the Netherlands, November 2020–March 2021. Euro Surveill. 2021;26(36):pii=2100792. https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2021.26.36.2100792
In March 2021, approximately one in five people in the Netherlands reported having no intention or being unsure of whether to get vaccinated against COVID-19.
13 September
Shen K, Loomer L, Abrams H, et al. Estimates of COVID-19 Cases and Deaths Among Nursing Home Residents Not Reported in Federal Data. JAMA Netw Open September 9, 2021;4(9):e2122885. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2784031
In this cross-sectional study of 15,307 US nursing homes, approximately 44% of COVID-19 cases and 40% of COVID-19 deaths that occurred before the start of reporting were not reported in the first NHSN submission in sample states, suggesting there were more than 68,000 unreported cases and 16,000 unreported deaths nationally.
11 September
Wilkinson E, Giovanetti M, Tegally H, et al. A year of genomic surveillance reveals how the SARS-CoV-2 pandemic unfolded in Africa. Science Sepember 9, 2021. https://www.science.org/doi/10.1126/science.abj4336
Phylogeographic reconstruction of (past) viral dissemination patterns, suggesting a strong epidemiological linkage between Europe and Africa, with 64% of detectable viral imports into Africa originating in Europe and 41% of detectable viral exports from Africa landing in Europe. Strong conclusion: “If the pandemic is not controlled in Africa, we may see the production of vaccine escape variants that may profoundly affect the population in Africa and across the world.”
7 September
Kleynhans J, Tempia S, Wolter N, et al. SARS-CoV-2 seroprevalence in a rural and urban household cohort during first and second waves of infections, South Africa, July 2020–March 2021. Emerg Infect Dis September 3, 2021. https://wwwnc.cdc.gov/eid/article/27/12/21-1465_article
The authors assessed SARS-CoV-2 seroprevalence in 1211 persons living in 2 diverse communities in South Africa and show, not surprisingly, that laboratory-confirmed cases reported from study districts greatly underestimate the actual prevalence. At baseline, seroprevalence was 1% in a rural community and 15% in an urban community, increasing to 7% and 27%, respectively, after the first wave, by March 2021. After the second wave, seroprevalence was 26% (rural) and 41% (urban).
5 September
Matthias J, Patrick S, Wiringa A, et al. Epidemiologically Linked COVID-19 Outbreaks at a Youth Camp and Men’s Conference — Illinois, June–July 2021. MMWR August 31, 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7035e4.htm?s_cid=mm7035e4_w
On June 30, 2021, the Illinois Department of Public Health reported two events sponsored by the same organization: a 5-day overnight church camp for persons aged 14–18 years and a 2-day men’s conference. Believe it or not, neither COVID-19 vaccination nor COVID-19 testing was required before either event. As of August 13, a total of 180 confirmed and probable cases had been identified among attendees at the two events and their close contacts. Among 122 primary cases, 104 (85%) were in persons not fully vaccinated, and 18 (15%) were in fully vaccinated persons. Eight of 38 (21%) close contacts of the 18 fully vaccinated persons subsequently became infected with SARS-CoV-2.
4 September
Brooks YM, Gryskwicz B, Sheehan S, Piers S, Mahale P, McNeil S, et al. Detection of SARS-CoV-2 in wastewater at residential college, Maine, USA, August–November 2020. Emerg Infect Dis August 31, 2021. https://wwwnc.cdc.gov/eid/article/27/12/21-1199_article
Wastewater surveillance may help to identify outbreaks. Cumulative increases of > 1 log10 SARS-CoV-2 RNA in consecutive 24-hour composite samples preceded outbreaks. For 76% of cases at a school, RNA was identified in grab samples from residence halls < 7 days before case discovery.
3 September
Soucy JP, Ghasemui A, Sturrock SL, et al. Trends in Interregional Travel to Shopping Malls and Restaurants Before and After Differential COVID-19 Restrictions in the Greater Toronto Area. JAMA Netw Open August 21, 2021; 4(8):e2123139. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2783631
Heterogeneous restrictions or partial lockdowns do not make sense: people/viruses just go shopping somewhere else. In this study from Canada, lockdowns in the urban center were associated with reduced overall visits to shopping malls and restaurants by residents but were not associated with decreased travel to these businesses in peripheral regions, where restrictions permitted indoor dining and shopping for non-essential businesses. The authors observed a large increase in visits to shopping malls in the peripheral regions by residents of the urban center in the week following the lockdown.
Keehner J, Horton LE, Binkin NJ, et al. Resurgence of SARS-CoV-2 Infection in a Highly Vaccinated Health System Workforce. NEJM September 1, 2021. https://www.nejm.org/doi/full/10.1056/NEJMc2112981?query=featured_home
Rapidly increasing cases among the workforce of the University of California San Diego Health, coinciding with the dominance of the Delta variant, and including cases among fully vaccinated persons. However, the increase was also coincident with the end of California’s mask mandate at the same time.
31 August
Kephart JL, Delclòs-Alió X, Rodríguez DA, et al. The effect of population mobility on COVID-19 incidence in 314 Latin American cities: a longitudinal ecological study with mobile phone location data. Lancet Dig Health August 26, 2021. https://doi.org/10.1016/S2589-7500(21)00174-6
Interventions to promote social distancing that target specific areas within cities might substantially mitigate SARS-CoV-2 transmission while reducing regional or citywide disruption. A 10% lower weekly mobility was associated with 8.6% (95% CI 7.6–9.6) lower incidence of COVID-19 in the following week.
28 August
Pei S, Yamana TK, Kandula S, et al. Burden and characteristics of COVID-19 in the United States during 2020. Nature August 27, 2021. https://doi.org/10.1038/s41586-021-03914-4
Roughly one third of the US population has been infected. The national infection fatality rate during the latter half of 2020 hovers around 0.30%, well above estimates for both seasonal influenza (< 0.08%) and the 2009 influenza pandemic (0.0076%).
27 August
Petti S. Undetected and relatively sustained SARS-CoV-2 circulation worldwide during the year 2019. Clinical Infectious Diseases August 2021, ciab727, https://doi.org/10.1093/cid/ciab727
A brief summary on current data suggesting the hypothesis that in 2019, SARS-CoV-2 circulation was already relatively sustained in Europe and America.
24 August
Moritz S, Gottschick C, Horn J, et al. The risk of indoor sports and culture events for the transmission of COVID-19. Nat Commun August 2021, 12, 5096. https://www.nature.com/articles/s41467-021-25317-9
The authors conducted an “experimental” pop concert (music was mainstream) on August 22nd 2020, with a total of 1212 individuals in the Leipzig Arena, Germany. They conclude that with an effective ventilation system, indoor mass gathering events with suitable hygiene practices have a very small, if any, effect on epidemic spread. If you are interested in the ventilation system in the arena: the inlet air is blown in laterally on the east- and west side by jet nozzles. https://static-content.springer.com/esm/art%3A10.1038%2Fs41467-021-25317-9/MediaObjects/41467_2021_25317_MOESM7_ESM.mp4
23 August
Madsen JR, Nielsen JPS, Fogh K, et al. Anti-SARS-CoV-2 Seropositivity Among Medical Students in Copenhagen. Open Forum Infectious Diseases 2021, publshed 19 August. Full text: https://academic.oup.com/ofid/article/8/8/ofab273/6354577
“Medical students have the highest reported seropositivity (34.58%) in the Danish health care system. In this cohort of students at University of Copenhagen, seropositivity was associated with social behavior markers and, to a lesser extent, with self-reported contact with SARS-CoV-2-infected patients.”
21 August
Zhang S. The Coronavirus Is Here Forever. This Is How We Live With It. The Atlantic 2021, published 17 August. Full text: https://www.theatlantic.com/science/archive/2021/08/how-we-live-coronavirus-forever/619783
The path from COVID-19 to the common cold.
20 August
Kupferschmidt K. Evolving Threat. Science 2021, publshed 19 August. Full text: https://www.sciencemag.org/news/2021/08/new-sars-cov-2-variants-have-changed-pandemic-what-will-virus-do-next
“New SARS-CoV-2 variants have changed the pandemic. What will the virus do next?”
19 August
Wadman M. A grim warning from Israel: Vaccination blunts, but does not defeat Delta. Science 2021, published 16 August. Full text: https://www.sciencemag.org/news/2021/08/grim-warning-israel-vaccination-blunts-does-not-defeat-delta
“Israel, which has led the world in launching vaccinations and in data gathering, is confronting a surge of COVID-19 cases that officials expect to push hospitals to the brink. Nearly 60% of gravely ill patients are fully vaccinated.”
17 August
Khullar D. How Will the Coronavirus Evolve? The New Yorker 2021, published 11 August. Full text: https://www.newyorker.com/science/annals-of-medicine/how-will-the-coronavirus-evolve
A nice read about Lenski’s Long-Term Evolution Experiment and possible SARS coronavirus citrate moments, that exceptionally rare, profoundly consequential evolutionary leaps can happen.
16 August
OHA 20210805. COVID-19 Monthly Report | Oregon’s Weekly Surveillance Summary. Oregon Health Authority 2021, published 5 August. Full text: https://www.oregon.gov/oha/covid19/Documents/DataReports/Breakthrough-Report-08-2021.pdf
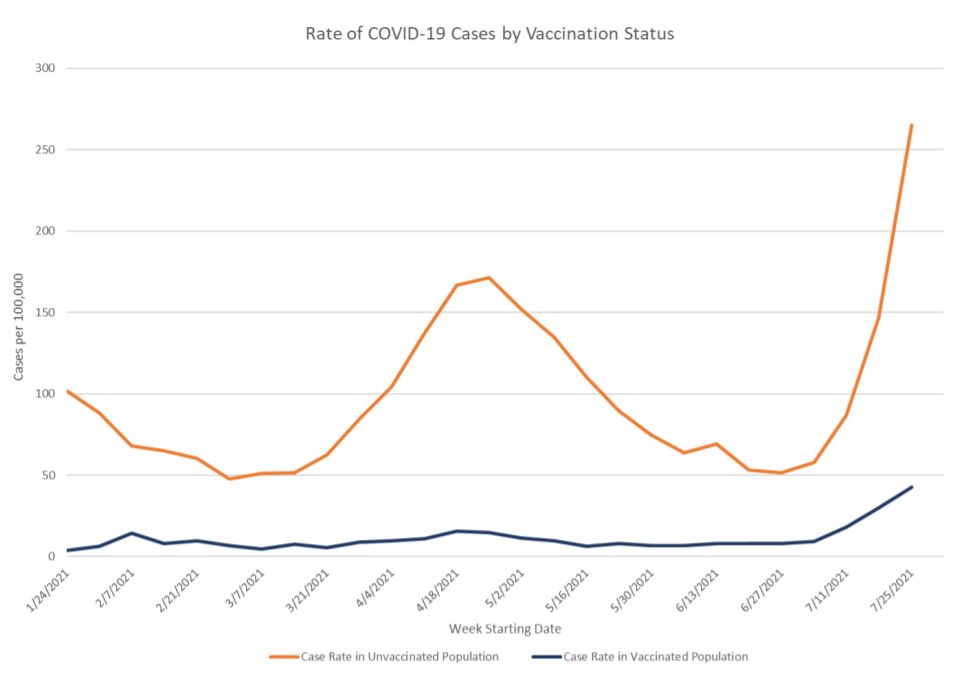
In Oregon (US), the beginning of the 4th wave of the pandemic is that it is a wave of the unvaccinated. In July 2021, 81% of 12,514 COVID-19 cases were among unvaccinated people, as were 82% of COVID-19-related deaths. Conclusion: “Although the number of vaccine breakthrough cases is increasing, they are very small when compared to the more than 2.3 million people who have completed their COVID-19 vaccination.”
Leatherby L. See How Vaccines Can Make the Difference in Delta Variant’s Impact. The New York Times 2021, published 12 August. Infographic: https://www.nytimes.com/interactive/2021/08/12/science/covid-delta-breakthrough.html
As the number of vaccinated people increases, so will the number of breakthrough cases. This doesn’t mean that our vaccines are ineffective. See this very instructional infographic which modeled Delta-driven COVID outbreaks in two communities, one with a high vaccination rate and another with a low rate. Their levels of serious illness and death were starkly different.
15 August
Rozier G. Guadeloupe. CovidTracker 2021, update 13 August. Web page: https://covidtracker.fr/dashboard-departements/?dep=971
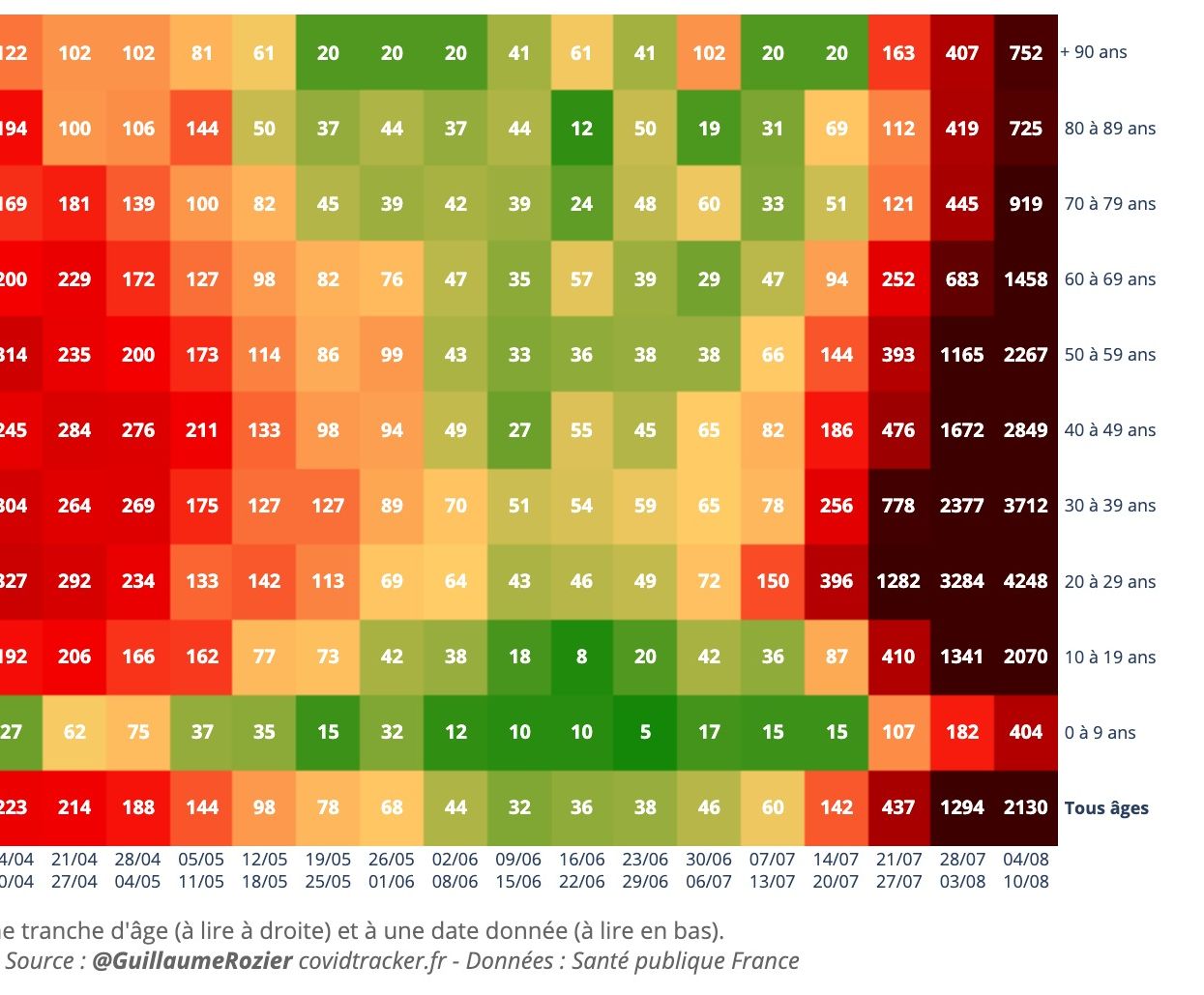
Guadeloupe – and to a lesser extent her sister island Martinique (see Google Maps) – are a telling picture of the Delta variant entering a population where less than 20% had their first COVID-19 vaccine shot. For the week 4-10 August, the cumulative incidence in young adults aged 20 to 29 years was… 4248! For these islands, tourism specialists predict a decline in visitor numbers in the next high season (December 2021 – April 2021).
Copyright: Guillaume Rozier – https://twitter.com/GuillaumeRozier
Yong E. How the Pandemic Now Ends. The Atlantic 2021, published 12 August. Full text: https://www.theatlantic.com/health/archive/2021/08/delta-has-changed-pandemic-endgame/619726/
Just one of several excellent quotes, “Here, then, is the current pandemic dilemma: Vaccines remain the best way for individuals to protect themselves, but societies cannot treat vaccines as their only defense. And for now, unvaccinated pockets are still large enough to sustain Delta surges, which can overwhelm hospitals, shut down schools, and create more chances for even worse variants to emerge.”
12 August
Rocklöv J, Liu Y. The reproductive number of the Delta variant of SARS-CoV-2 is far higher compared to the ancestral SARS-CoV-2 virus. J Travel Med 2021, published 9 August. Full text: https://doi.org/10.1093/jtm/taab124
Don’t throw your masks away, even if you are vaccinated. Here, the authors summarize 5 studies that estimate the basic reproductive number for the Delta variant ranging from 3.2 to 8, with a mean of 5.08. This is almost double the R0 of the historical strain which is 2.79. Vaccination alone may not be sufficient until well into 2022.
11 August
Wallace-Wells D. Too Many People Are Dying Right Now. “It’s hard to look at these indicators and feel at all optimistic,” explains scientist Eric Topol. Intelligencer 2021, published 8 August. Full text: https://nymag.com/intelligencer/2021/08/too-many-people-are-dying-of-covid-19-right-now.html
There is much uncertainty about how the Delta wave will evolve in the United States. An interview with Eric Topol, director of the Scripps Research Translational Institute.
29 July
Bindman P. Who has been hit hardest by the UK’s third wave of Covid-19? New Statesman 2021, published 21 July. Full text: https://www.newstatesman.com/politics/health/2021/07/who-has-been-hit-hardest-uk-s-third-wave-covid-19
How the UK’s vaccine roll-out has thus far reduced the number of COVID-19 deaths. What about the coming weeks?
24 July
Ito K, Piantham C, Nishiura H. Predicted dominance of variant Delta of SARS-CoV-2 before Tokyo Olympic Games, Japan, July 2021. Euro Surveill. 2021 Jul;26(27):2100570. PubMed: https://pubmed.gov/34240695. Full-text: https://doi.org/10.2807/1560-7917.ES.2021.26.27.2100570
In many countries, the Delta variant (B.1.671.2) has already replaced other variants. The authors show that in Japan, the replacement is likely to happen mostly before the start of the Tokyo Olympic Games on 23 July 2021. A substantial number of international visitors might be exposed and help spread the Delta variant around the world.
20 July
Guimarães RM, Portela MC, Villela DAM, Matta GC, de Freitas CM. Younger Brazilians hit by COVID-19 – What are the implications? Lancet Regional Health 2021, published 14 July. Full text: https://doi.org/10.1016/j.lana.2021.100014
New variants and incomplete vaccination will lead to increasing numbers of young and middle-aged adults in intensive care units. In the months ahead, how far will the “youthening of the pandemic” go? In Brazil, among patients who died from COVID-19, the median age has dropped 13 years since the beginning of 2021.
17 July
Kimihito I, Chayada P, NHiroshi N. Predicted dominance of variant Delta of SARS-CoV-2 before Tokyo Olympic Games, Japan, July 2021. Euro Surveill. 2021;26(27):pii=2100570. https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2021.26.27.2100570
It is just a matter of time for the Delta variant to replace other variants in Japan. This study shows that the replacement is likely to happen mostly before the start of the Tokyo Olympic Games on 23 July 2021.
15 July
Kofman A, Kanto R, Adashi EY. Potential COVID-19 Endgame Scenarios. JAMA July 8, 2021. https://jamanetwork.com/journals/jama/fullarticle/2781945
Eradication, elimination, cohabitation, or conflagration? This viewpoint describes four potential scenarios that may constitute the resolution of the COVID-19 pandemic.
24 June
Kwon S, Joshi AD, Lo CH. et al. Association of social distancing and face mask use with risk of COVID-19. Nat Commun Jun 21, 2021, 12, 3737. https://www.nature.com/articles/s41467-021-24115-7
Individuals living in communities with the greatest social distancing had a 31% lower risk of predicted COVID-19 compared with those living in communities with poor social distancing. Self-reported ‘always’ use of face mask was associated with a 62% reduced risk of predicted COVID-19 even among individuals living in a community with poor social distancing.
23 June
Whaley CM, Cantor J, Pera M, et al. Assessing the Association Between Social Gatherings and COVID-19 Risk Using Birthdays. JAMA Intern Med June 21, 2021. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2781306?resultClick=1
Yes, there is an association between household birthdays, which likely correspond to informal social gatherings, and COVID-19. Among the 2.9 million households in the study, in the top 10% of counties in COVID-19 prevalence, households with a birthday in the 2 weeks prior had 8.6 more diagnoses per 10,000 individuals compared with households without a birthday in the 2 weeks prior. The relative increase was 31% of county-level prevalence and was even larger in magnitude in households that had a recent child’s (vs adult’s) birthday.
21 June
García CR, Iftimi A, Briz-Redón A, et al. Trends in Incidence and Transmission Patterns of COVID-19 in Valencia, Spain. JAMA Netw Open June 18, 2021; 4(6):e2113818. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2781191?resultClick=1
The major observation of this epidemiological cohort study of 2646 patients with COVID-19 was that the neighborhood where the COVID-19 testing facility was located also had the highest number of total connections (both inbound and outbound). Thus, hospitals with a testing facility might become a major contributor to local spread.
15 June
Dinakarpandian D, Sullivan KJ, Thadaney-Israni S, et al. International Medical Graduate Physician Deaths From COVID-19 in the United States. JAMA Netw Open June 11, 2021;4(6):e2113418. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2780929?resultClick=1
In this case series, the proportion of international medical graduates among 132 physicians (many of whom worked in primary care) who died from COVID-19 was higher than their national proportion among practicing US physicians.
13 June
Milman O, Yelin I, Aharony N et al. Community-level evidence for SARS-CoV-2 vaccine protection of unvaccinated individuals. Nat Med June 10, 2021. https://doi.org/10.1038/s41591-021-01407-5
Vaccination provides cross-protection to unvaccinated individuals in the community: this groundbreaking study from Israel shows that on average, for each 20 percentage points of individuals who are vaccinated in a given population, the positive test fraction for the unvaccinated population decreased approximately twofold.
12 June
Payne AB, Gilari Z, Godfred-Cato S, et al. Incidence of Multisystem Inflammatory Syndrome in Children Among US Persons Infected With SARS-CoV-2. JAMA Netw Open June 10, 2021;4(6):e2116420. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2780861?resultClick=1
MIS-C incidence was 5.1 persons per 1,000,000 person-months and 316 persons per 1,000,000 SARS-CoV-2 infections in persons younger than 21 years.
8 June
Xiao X, Newman C, Buesching CD, et al. Animal sales from Wuhan wet markets immediately prior to the COVID-19 pandemic. Sci Rep June 7, 2021, 11, 11898. https://www.nature.com/articles/s41598-021-91470-2#Bib1
Here the authors document 47,381 individuals from 38 species, including 31 protected species sold between May 2017 and November 2019 in Wuhan’s markets. They also note the poor conditions under which the animals were kept prior to sale. No pangolins (or bats) were traded, supporting that pangolins were not likely the spillover host at the source of the pandemic.
6 June
Lash RR, Moonan PK, Byers BL, et al. COVID-19 Case Investigation and Contact Tracing in the US, 2020. JAMA Netw Open June 3, 2021. 2021;4(6):e2115850. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2780568?resultClick=1
In this cross-sectional study of US local COVID-19 surveillance data, contact tracing had suboptimal impact on SARS-CoV-2 transmission, largely because two out of every three cases were either not reached for interview or had named no contacts when interviewed.
5 June
Hay JA, Kennedy-Shaffer L, Kanjilal S, et al. Estimating epidemiologic dynamics from cross-sectional viral load distributions. Science 03 Jun 2021: eabh0635. https://science.sciencemag.org/content/early/2021/06/02/science.abh0635
Distribution of observed Ct values has varied over the course of the current pandemic. This study suggests that this can be explained as an epidemiologic phenomenon, without invoking any change in individual level viral kinetics or testing practices. Properties of the population level Ct distribution strongly correlate with estimates for the effective reproductive number or growth rate in real world settings. In other words: Ct values from single or successive cross-sectional samples of RT-qPCR data can be used to estimate the epidemic trajectory without requiring additional information from test positivity rates or serial case counts.
3 June
Patel MD, Rosenstrom E, Ivy JS, et al. Association of Simulated COVID-19 Vaccination and Nonpharmaceutical Interventions With Infections, Hospitalizations, and Mortality. JAMA Netw Open June 1, 2021;4(6):e2110782. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2780539
Interesting finding: compared with more efficacious vaccines with lower population coverage, as NPIs are removed, higher vaccination coverage with less efficacious vaccines can contribute to a larger reduction in risk of SARS-CoV-2 infection.
1 June
Liu Y, Wang Z, Rader B, et al. Associations between changes in population mobility in response to the COVID-19 pandemic and socioeconomic factors at the city level in China and country level worldwide: a retrospective, observational study. Lancet Digital Health, June 1, 2021. Volume 3, ISSUE 6, e349-e359. https://www.thelancet.com/journals/landig/article/PIIS2589-7500(21)00059-5/fulltext
Using empirical data from 358 cities in China and 121 countries globally, the authors analyzed population mobility data before and after emergency responses were introduced. Several factors were associated with reduced intra-city movement intensity, including a high proportion of people in age groups between 20 and 39 years, socioeconomic factors (ie, education level), and COVID-19-related factors (ie, lockdown status and number of COVID-19 cases). A higher sociodemographic index showed a greater reduction in mobility.
31 May
García-García D, Vigo MI, Fonfría ES, et al. Retrospective methodology to estimate daily infections from deaths (REMEDID) in COVID-19: the Spain case study. Sci Rep 11, 11274 (2021). https://www.nature.com/articles/s41598-021-90051-7
During the first wave, infection numbers were largely underestimated in Spain. The authors propose a retrospective methodology to estimate daily infections from daily deaths because deaths are usually more accurately documented. They estimate that probable daily infections during the first wave were between 35 and 42 times higher than those officially documented on 14 March, when the national government decreed a national lockdown and still 9 times more than those documented by the updated version of the official data.
29 May
Ganegoda NC, Wijaya KP, Amadi M, et al. Interrelationship between daily COVID-19 cases and average temperature as well as relative humidity in Germany. Sci Rep 11, 11302, May 28, 2021). https://doi.org/10.1038/s41598-021-90873-5
Well… please correct us if we are wrong: reported daily COVID-19 cases correlated negatively with the average temperature and positively with the average relative humidity. Correct?
However, temperature can only predict incident cases during hot (summer) and cold seasons (winter), not during transitional seasons (spring and fall). Relative humidity, on the other hand, is less likely to predict falling cases during hot seasons.
26 May
Wilson N, Baker MG, Blakely T, et al. Estimating the impact of control measures to prevent outbreaks of COVID-19 associated with air travel into a COVID-19-free country. Sci Rep May 24, 2021, 11, 10766. https://www.nature.com/articles/s41598-021-89807-y
This modelling study suggests that the risk of an outbreak in a previously COVID-19-free country is extremely dependent on the source country of the incoming travelers. In some countries, the risk could potentially be reduced to tolerable levels with a package of multi-layered interventions (particularly with repeated testing and mask use) and no quarantine. Nevertheless, quarantine is likely to remain important when the source country has high disease burden.
Gettings J, Czarnik M, Morris E, et al. Mask Use and Ventilation Improvements to Reduce COVID-19 Incidence in Elementary Schools — Georgia, November 16–December 11, 2020. MMWR Morb Mortal Wkly Rep 21 May 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7021e1.htm
Representatives from 169 (11.6%) of 1461 schools in 51 Georgia counties completed a survey and also had available COVID-19 case data. COVID-19 incidence was 37% lower in schools that required teachers and staff members to use masks and 39% lower in schools that improved ventilation. Ventilation strategies associated with lower school incidence included dilution methods alone (35% lower incidence) or in combination with filtration methods (48% lower incidence).
25 May
Hodgson D, Flasche S, Jit M, et al. The potential for vaccination-induced herd immunity against the SARS-CoV-2 B.1.1.7 variant. Euro Surveill May 20, 2021. 26(20):pii=2100428. https://doi.org/10.2807/1560-7917.ES.2021.26.20.2100428
This brilliant modeling study suggests that if highly transmissible variants become dominant in areas with low seroprevalence, control of infection by vaccination, in the absence of non-pharmaceutical interventions, may only be achievable with a vaccine effectiveness against infectiousness of ≥ 80% – as suggested by early data for mRNA vaccines – extended to the full population, including children.
Lanier WA, Babitz KD, Collingwood A, et al. COVID-19 Testing to Sustain In-Person Instruction and Extracurricular Activities in High Schools — Utah, November 2020–March 2021. MMWR Morb Mortal Wkly Rep. ePub: 21 May 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7021e2.htm?s_cid=mm7021e2_w
Listen up, education policymakers: Utah implemented two high school COVID-19 testing programs to sustain in-person instruction and extracurricular activities. During November 30, 2020–March 20, 2021, of 59,552 students who received testing, 1886 (3.2%) had a positive result. These programs facilitated the completion of approximately 95% of high school extracurricular competition events and saved an estimated 109,752 in-person instruction student-days.
24 May
Le Vu, S., Jones, G., Anna, F. et al. Prevalence of SARS-CoV-2 antibodies in France: results from nationwide serological surveillance. Nat Commun May 21, 12, 3025. https://www.nature.com/articles/s41467-021-23233-6
The first wave in France. Testing 11,000 residual specimens for anti-SARS-CoV-2 IgG and neutralizing antibodies, the authors found nationwide seroprevalence of 0.41% mid-March, 4.14% mid-April and 4.93% mid-May 2020. The authors infer that as of 17 May 2020, only 1 in 24 cumulative infections was reported as a confirmed case. Overall infection fatality rate (IFR) was estimated at 0.84% and increased exponentially with age, peaking in those ≥ 80 years old at 9.70%.
22 May
Chu DKW, Gu H, Chang LDJ, Cheuk SSY, Gurung S, Krishnan P, et al. SARS-CoV-2 superspread in fitness center, Hong Kong, China, March 2021. Emerg Infect Dis. 2021 Aug [date cited]. https://doi.org/10.3201/eid2708.210833
An asymptomatic 27-year-old male fitness trainer with a positive PCR. About 300 visitors were tested and 101 cases were confirmed (7 staff members and 94 customers). Mask wearing during exercise was not compulsory by law at the time of this outbreak.
17 May
Holmdahl I, Kahn R, Hay JA, et al. Estimation of Transmission of COVID-19 in Simulated Nursing Homes With Frequent Testing and Immunity-Based Staffing. JAMA Netw Open May 14, 2021, 4(5):e2110071. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2779870
Frequent and rapid testing! This decision analytical modeling study has evaluated COVID-19 transmission in nursing homes associated with contact-targeted interventions and testing. The testing strategy associated with the greatest estimated reduction in infections was daily antigen testing, indicating that faster results should be prioritized over higher sensitivity.
14 May
Guagliardo SA, Prasad PV, Rodriguez A, et al. Cruise ship travel in the era of COVID-19: A summary of outbreaks and a model of public health interventions. Clinical Infectious Diseases May 12, 2021, ciab433, https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab433/6274545
SARS-CoV-2 outbreaks on cruises in US waters or carrying US citizens: from January 19 to April 16, 2020, 89 voyages on 70 ships had known outbreaks. There were 1669 SARS-CoV-2 infections and 29 confirmed deaths. Mathematical models showed that 7-day voyages had about 70% fewer cases than 14-day voyages. On 7-day voyages, the most effective interventions were reducing the number of individuals onboard (43-49%) and testing passengers and crew (42-43%). Of note, no single intervention or combination eliminated transmission.
9 May
Nunes MC, Baillie VL, Kwatra G, et al. SARS-CoV-2 infection among healthcare workers in South Africa: a longitudinal cohort study. Clinical Infectious Diseases 05 May 2021, ciab398, https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab398/6265294
From April to September 2020, 35% of 396 HCWs at Chris Hani Baragwanath Hospital, South Africa had PCR-confirmed SARS-CoV-2 infection, an additional 27 infections were identified by serology. HCWs in the Internal Medicine department had the highest rate of infection (62%).
5 May
Hilt EE, Boocock J, Trejo M, et al. Retrospective Detection of SARS-CoV-2 in Symptomatic Patients prior to Widespread Diagnostic Testing in Southern California. Clin Inf Dis May 3, 2021, ciab360, https://doi.org/10.1093/cid/ciab360
The authors found SARS-CoV-2 in 7 specimens from 6 patients dating back to mid-January, indicating community spread of SARS-CoV-2 in the Los Angeles area well before widespread diagnostic testing was being performed in early 2020.
4 May
Tan AX, Hinman JA, Magidf HS, et al. Association Between Income Inequality and County-Level COVID-19 Cases and Deaths in the US. JAMA Netw Open. May 3, 2021. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2779417?resultClick=1
This ecological cohort study found that there was a positive correlation between Gini coefficients (a measure of unequal income distribution) and county-level COVID-19 cases and deaths during the study period. Of note, the association varied over time and was strongest in the summer months of 2020.
3 May
Wiens KE, Mawien PN, Rumunu J, Slater D, Jones FK, Moheed S, et al. Seroprevalence of severe acute respiratory syndrome coronavirus 2 IgG in Juba, South Sudan, 2020. Emerg Infect Dis April 27, 2021 Jun [date cited]. https://wwwnc.cdc.gov/eid/article/27/6/21-0568_article
Relatively few coronavirus cases and deaths have been reported from sub-Saharan Africa. After performing a huge cross-sectional survey in South Sudan (August–September 2020), the authors estimate that 38% (95% CI: 32%–47%) of the population had been infected with SARS-CoV-2. For each PCR–confirmed SARS-CoV-2 infection officially reported, 103 infections went unreported.
Feder KA, Pearlowitz M, Goode A, et al. Linked Clusters of SARS-CoV-2 Variant B.1.351 — Maryland, January–February 2021. MMWR Morb Mortal Wkly Rep 2021;70:627–631. https://www.cdc.gov/mmwr/volumes/70/wr/mm7017a5.htm?s_cid=mm7017a5_w#suggestedcitation
The first clusters of B.1.351 infections in the US with no identified link to international travel. The two linked clusters included 17 patients. Four cases were sequenced; all had the B.1.351 variant.
2 May
Carter RL, Rose D, Sabo R, et al. Widespread SARS-CoV-2 Transmission Among Attendees at a Large Motorcycle Rally and their Contacts, 30 US Jurisdictions, August–September, 2020. Clinical Infectious Diseases 29 April 2021, ciab321, https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab321/6257584
A major event, the Sturgis Motorcycle Rally, held in Meade County, South Dakota, August 7–16, 2020, with approximately 462,000 persons attending a variety of outdoor and indoor activities. South Dakota had implemented few restrictions and there were no state, county, or city mask mandates in effect. Attendance at the rally led to widespread SARS-CoV-2 transmission to 463 people in 30 jurisdictions, with 17 jurisdictions reporting subsequent transmission to 186 household and workplace contacts (it is likely that the true numbers are largely underestimated). No comment.
30 April
Oliu-Barton M, Pradelski BS, Aghion OP, et al. SARS-CoV-2 elimination, not mitigation, creates best outcomes for health, the economy, and civil liberties. April 28, 2021. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00978-8/fulltext
See title. “Living with the virus“ is not a good idea. And will not work. Important comment, good arguments. Evidence suggests that countries that opt for rapid action to eliminate SARS-CoV-2—with the strong back-up of their inhabitants—also better protect their economies and minimize restrictions on civil liberties compared to those that strive for mitigation.
27 April
Somekh I, Boker KL, Shohat T, et al. Comparison of COVID-19 Incidence Rates Before and After School Reopening in Israel. JAMA Netw Open April 26, 2021. 2021; 4(4):e217105. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2778940?resultClick=1
This study suggests that children aged 0 to 9 years did not have substantial rates of SARS-CoV-2 infection during school attendance periods, and it may be assumed that they did not have a substantial role in COVID-19 spread either during this period. Therefore, resuming school for this age group when lockdown was relaxed appears to have been safe for them.
26 April
Mallapaty S. India’s massive COVID surge puzzles scientists. Nature NEWS, April 21, 2021. https://www.nature.com/articles/d41586-021-01059-y
The virus is spreading faster than ever before in the country despite previous high infection rates in megacities, which should have conferred some protection. Smriti Mallapaty summarizes the current knowledge. It remains unclear whether the surge is due to the new variant B.1.617 or due to a fully open society where people were mixing and moving and travelling. Or both.
Brief summary on B.1.617: https://www.sciencemediacentre.org/expert-reaction-to-cases-of-variant-b-1-617-the-indian-variant-being-investigated-in-the-uk/
Watson OJ, Alhaffar M, Mehchy Z, et al. Leveraging community mortality indicators to infer COVID-19 mortality and transmission dynamics in Damascus, Syria. Nat Commun 12, 2394 (2021). https://www.nature.com/articles/s41467-021-22474-9
What about Syria? By 2 September, the authors estimate that by September 2, 2020, 4380 (95% CI: 3250 – 5550) COVID-19 deaths in Damascus may have been missed, with 39.0% (95% CI: 32.5% – 45.0%) of the population in Damascus estimated to have been infected.
25 April
Moghadas SM, Fitzpatrick MC, Shoukat A, et al. Simulated Identification of Silent COVID-19 Infections Among Children and Estimated Future Infection Rates With Vaccination. JAMA Netw Open April 23, 2021; 4(4):e217097. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2779052?resultClick=1
In this simulation modeling study of a synthetic US population, in the absence of vaccine availability for children, a targeted approach to rapidly identify silent COVID-19 infections in this age group was estimated to significantly mitigate disease burden. Without these measures, vaccination of adults is unlikely to contain outbreaks in the near term.
24 April
Panovska-Griffiths J, Kerr CC, Waites W et al. Modelling the potential impact of mask use in schools and society on COVID-19 control in the UK. Sci Rep April 22, 2021, 11, 8747. https://www.nature.com/articles/s41598-021-88075-0
This modelling study from the UK shows that mandating the use of masks in secondary schools would not be sufficient to prevent a COVID-19 resurgence in late 2020. Assuming test-trace-isolate (TTI) levels from August 2020 and no changes in the virus’s transmissibility, adoption of masks would have reduced the predicted size of a second wave, but preventing it would have required 68% or 46% of those with symptoms to seek testing (assuming masks’ effective coverage 15% or 30% respectively). With masks in community settings but not secondary schools, the required testing rates increase to 76% and 57%.
20 April
Gettings JR, Gold JA, Kimball A, et al. SARS-CoV-2 transmission in a Georgia school district — United States, December 2020–January 2021. Clinical Infectious Diseases, April 17, 2021, ciab332. https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab332/6232104?searchresult=1
During December 1, 2020–January 22, 2021, 86 index cases and their close contacts in schools were identified. Of 679 contacts, 59 (9%) tested positive. Highest secondary attack rates were observed in indoor, high-contact sports settings (24%) and staff meetings/lunches (18%).
Di Domenico L, Sabbatini CE, Pullano G, et al. Impact of January 2021 curfew measures on SARS-CoV-2 B.1.1.7 circulation in France. Euro Surveill. 2021;26(15):pii=2100272. https://doi.org/10.2807/1560-7917.ES.2021.26.15.2100272
Curfew alone is not enough. The authors estimate that curfew measures allowed hospitalizations to plateau by decreasing transmission of the historical strains while B.1.1.7 continued to grow. Without progressively strengthened social distancing, a rapid surge of hospitalizations is expected, despite the foreseen increase in vaccination rhythm.
12 April
Matthias J, Charboneau T, Schaffer C, et al. Notes from the Field: COVID-19 Case Investigation and Contact Tracing Program — Spirit Lake Tribe, North Dakota, September–November 2020. MMWR Morb Mortal Wkly Rep 2021;70:533–534. https://www.cdc.gov/mmwr/volumes/70/wr/mm7014a4.htm?s_cid=mm7014a4_w
The Spirit Lake sovereign nation in North Dakota is home to approximately 7,500 members of the Spirit Lake Tribe. From September 29–November 20, 2020, a total of 317 infected persons and 667 close contacts were reported; 129 (19.3%) of these close contacts received a subsequent COVID-19 diagnosis. A tribally managed COVID-19 case investigation and contact tracing program effectively reached tribal members and contributed to timely case and contact management. Good news, because control of the pandemic may be possible, even in hard-to-reach populations (if you involve them).
11 April
Pathela P, Crawley A, Weiss D, et al. Seroprevalence of SARS-CoV-2 following the largest initial epidemic wave in the United States: Findings from New York City, May 13-July 21, 2020. J Inf Dis 09 April 2021, jiab200, https://academic.oup.com/jid/advance-article/doi/10.1093/infdis/jiab200/6219118?searchresult=1
In this large serosurvey of 45,367 adult NYC residents during the first wave, seroprevalence was high, reaching 23.6% (95% CI: 23.2%-24.0%). As this was a convenience sample, however, it is possible that people who sought out testing perceived themselves to have been more likely to have been exposed to SARS-CoV-2. High seroprevalence (> 30%) was observed among Black and Hispanic individuals, people from high poverty neighborhoods, and people in health care or essential worker industry sectors.
7 April
Hippich M, Sifft P, Zapardiel-Gonzalo J, et al. A Public Health Antibody Screening Indicates a Marked Increase of SARS-CoV-2 Exposure Rate in Children during the Second Wave. Med April 02, 2021. https://www.cell.com/med/fulltext/S2666-6340(21)00121-5
In this large monitoring study from Bavaria, Germany, antibody frequencies in 2021 were eight-fold higher than those observed at the end of the first wave and remained three- to four-fold higher than the cumulative reported PCR positive frequencies in both pre-school and school children. Among the 413 PCR-positive children who completed questionnaires regarding symptoms, no symptoms were reported in 68% of antibody-positive pre-school children and in 52% of school children.
6 April
Hershow RB, Segaloff HE, Shockey AC, et al. Rapid Spread of SARS-CoV-2 in a State Prison After Introduction by Newly Transferred Incarcerated Persons — Wisconsin, August 14–October 22, 2020. MMWR Morb Mortal Wkly Rep April 2, 2021;70:478–482. https://www.cdc.gov/mmwr/volumes/70/wr/mm7013a4.htm?s_cid=mm7013a4_x
Limited testing resources and limited space for quarantine and medical isolation in a state prison: in 9 weeks (August 14–October 22), 869 (79.4%) of 1095 incarcerated persons and 69 (22.6%) of 305 staff members received positive test results for SARS-CoV-2.
Lewis NM, Salmanson AP, Price A, et al. Community-Associated Outbreak of COVID-19 in a Correctional Facility — Utah, September 2020–January 2021. MMWR Morb Mortal Wkly Rep April 2, 2021;70:467–472. https://www.cdc.gov/mmwr/volumes/70/wr/mm7013a2.htm?s_cid=mm7013a2_w
Same issue: a prison in Utah. An outbreak was introduced by a dental health care provider (DHCP) who had treated incarcerated persons (wearing an N95 mask as well as gown, gloves, and goggles) while asymptomatic. Outbreak spread was incredibly rapid, eventually affecting 1368 (52%!) of 2632 residents (with 31 hospitalizations and 12 deaths) as well as to an estimated 88 (16%) of 550 staff members. As of March 2, 2021, the outbreak was ongoing. According to the authors, screening of non-facility HCPs with rapid antigen tests (as well as testing incarcerated persons after receiving treatment) would have been a good idea.
5 April
Codreanu TA, Ngeh S, Trewin A, Armstrong PK. Successful control of an onboard COVID-19 outbreak using the cruise ship as a quarantine facility, Western Australia. Emerg Infect Dis 2021 May https://wwwnc.cdc.gov/eid/article/27/5/20-4142_article
Do you remember the Diamond Princess outbreak in early 2020? These guys here probably have done a better job, reporting on the successful use of a ship as a quarantine facility during the response to the outbreak on the MS Artania, docked in Western Australia. The 14-day quarantine regimen was based on established principles of outbreak management and experiences of outbreaks on cruise ships elsewhere. The attack rate in the crew was 3.3% (28/832) before quarantine commencement and 4.8% (21/441) during quarantine on board (remember Diamond Princess: 17%).
2 April
Naimark D, Mishra S, Barrett K. Simulation-Based Estimation of SARS-CoV-2 Infections Associated With School Closures and Community-Based Nonpharmaceutical Interventions in Ontario, Canada. JAMA March 31, 2021. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2777976?resultClick=1
The magnitude of the effect of schools being open on COVID-19 cases was substantially lower than the effect of community-based NPIs. These findings suggest that school closure be considered the last resort in the face of a resurgence of COVID-19, and that efforts should instead focus on widespread reduction of community transmission.
27 March
Salyer S, Maeda J, Sembuche S, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet 2021, published 24 March. Full text: https://doi.org/10.1016/S0140-6736(21)00632-2
Although the first wave of the COVID-19 pandemic progressed more slowly in Africa than the rest of the world, by December 2020, the second wave appeared to be much more aggressive with many more cases.
22 March
Rennert L, McMahan C, Kalbaugh CA, et al. Surveillance-based informative testing for detection and containment of SARS-CoV-2 outbreaks on a public university campus: an observational and modelling study. Lancet Child Adolescent Health March 19, 2021. https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(21)00060-2/fulltext
There is a strong need for testing strategies for mitigating SARS-CoV-2 spread on college and university campuses. The authors implemented a novel surveillance-based informative testing (SBIT) strategy for SARS-CoV-2 detection. In this setting, random testing is done to detect potential cluster outbreaks (eg, residence hall outbreaks). Upon detection of an outbreak, a portion of available tests the following day are allocated to the entire cluster. SBIT was effective in detecting and containing COVID-19 outbreaks and mitigating SARS-CoV-2.
21 March
Sandmann FG, Davies NG, Vassall A, et al. The potential health and economic value of SARS-CoV-2 vaccination alongside physical distancing in the UK: a transmission model-based future scenario analysis and economic evaluation. Lancet Inf Dis March 18, 2021. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(21)00079-7/fulltext
In a modelling study from the UK, highlighting the substantial health and economic value of introducing SARS-CoV-2 vaccination. Without the initial lockdown, vaccination, and increased physical distancing, the authors estimate that 3.1 million (0.84–4.5) deaths would occur in the UK over the next 10 years.
20 March
Pekar J, Worobey M, Moshiri N, et al. Timing the SARS-CoV-2 index case in Hubei province. Science 18 Mar 2021: eabf8003. DOI: 10.1126/science.abf8003. https://science.sciencemag.org/content/early/2021/03/17/science.abf8003
Shit happened in October/November 2019: employing a coalescent framework to combine retrospective molecular clock inference with forward epidemiological simulations, the authors determine here how long SARS-CoV-2 could have been circulating prior to its “official” recognition. Results define the period between mid-October and mid-November 2019 as the plausible interval when the first case of SARS-CoV-2 emerged in Hubei province.
15 March
van den Berg P, Schechter-Perkins EM, Jack RS, et al. Effectiveness of three versus six feet of physical distancing for controlling spread of COVID-19 among primary and secondary students and staff: A retrospective, state-wide cohort study. Clinical Infectious Diseases 10 March 2021, ciab230, https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab230/6167856?searchresult=1
Incident cases of SARS-CoV-2 in students and staff in Massachusetts public schools among districts with different physical distancing requirements did not differ, suggesting that the less physical distancing recommendation can be adopted in school settings without negatively impacting safety.
14 March
CMMID 202103. European COVID-19 Forecast hub. London School of Hygiene & Tropical Medicine and ECDC 2021. Website: https://covid19forecasthub.eu
The European COVID-19 Forecast hub aims to collate and meaningfully combine short-term forecasts of COVID-19 from across Europe in order to 1) improve situational awareness and 2) quantify the current trajectory of COVID-19 everywhere whilst acknowledging uncertainty.
Graphic
Mallapaty S. The search for animals harbouring coronavirus — and why it matters. Nature 2021, published 2 March. Full-text: https://www.nature.com/articles/d41586-021-00531-z
Monitoring pets, livestock and wildlife to see where SARS-CoV-2 could hide, and whether it might resurge.
Graphic
13 March
Sartorius B, Lawson AB, Pullan RL. Modelling and predicting the spatio-temporal spread of COVID-19, associated deaths and impact of key risk factors in England. Sci Rep 11, March 8, 2021, 5378. https://doi.org/10.1038/s41598-021-83780-2
This high resolution spatial–temporal model highlights differences in epidemic dynamics across small areas in England, emphasizing the importance of monitoring at a granular sub-national scale. A geographically staggered approach combined with enhanced community surveillance will be increasingly important.
Boffetta P, Violante F, Durando P, et al. Determinants of SARS-CoV-2 infection in Italian healthcare workers: a multicenter study. Sci Rep March 11, 2021, 5788. https://www.nature.com/articles/s41598-021-85215-4.pdf
The prevalence of infection ranged from 3% to 22%, and was correlated with that of the respective areas within Italy. Of note, there was a lack of a clear pattern in risk according to job categories.
12 March
Richard Q, Alizon S, Choisy M, et al. Age-structured non-pharmaceutical interventions for optimal control of COVID-19 epidemic. PLOS Computational Biology March 4, 2021. https://doi.org/10.1371/journal.pcbi.1008776
Complex models, trying to elucidate that countries with contrasted population age-structures and social or physical contacts may need different NPIs.
Bokharaie VS. A study on the effects of containment policies and vaccination on the spread of SARS-CoV-2. PLOS March 4, 2021. https://doi.org/10.1371/journal.pone.0247439
Same direction. A method to predict the spread of the SARS-CoV-2 in a population with a known age-structure, and then, to quantify the effects of various containment policies, including those policies that affect each age-group differently.
Mulenga LB, Hines JZ, Fwoloshi S, et al. Prevalence of SARS-CoV-2 in six districts in Zambia in July, 2020: a cross-sectional cluster sample survey. Lancet Global Health March 09, 2021. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(21)00053-X/fulltext
Almost 1 in 100 diagnosed: According to this first large cross-sectional cluster-sample survey of households in Africa (performed in July), the number of laboratory-confirmed cases reported in official statistics in Zambia underestimated SARS-CoV-2 infections by a factor of 92.
11 March
Agrawal S, Orschler L, Lackner S. Long-term monitoring of SARS-CoV-2 RNA in wastewater of the Frankfurt metropolitan area in Southern Germany. Sci Rep 11, 5372 (2021). https://www.nature.com/articles/s41598-021-84914-2
After monitoring the time course of the SARS-CoV-2 RNA concentration in raw sewage in the Frankfurt metropolitan area for several months, Shelesh Agrawal and colleagues believe that wastewater-based epidemiology has the potential to serve as an early warning system for SARS-CoV-2 infections and as a monitoring system to identify global hotspots.
Brault V, Mallein B, Rupprecht JF, et al. Group testing as a strategy for COVID-19 epidemiological monitoring and community surveillance. PLOS Computational Biology, March 4, 2021. https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1008726
Group testing could provide the means for regular and massive screenings. In this paper, the authors do not address any diagnostic problems—e.g. how to use a minimal number of tests to obtain an individual diagnostic—but rather focus on population-scale application of pooling.
10 March
Chen X, Chen Z, Azman AS, et al. Serological evidence of human infection with SARS-CoV-2: a systematic review and meta-analysis. Lancet March 08, 2021. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(21)00026-7/fulltext
After reviewing 404 (!) studies, the authors conclude that antibody-mediated herd immunity is far from being reached in most settings. Of note, the pooled infection-to-case ratio was similar between the region of the Americas (6.9, 95% CI: 2.7–17.3) and the European region (8.4, 95% CI: 6.5–10.7), but higher in India (56.5, 95% CI: 28.5–112.0), the only country in the South-East Asia region with data.
Leung K, Wu JT, Leung GM. Real-time tracking and prediction of COVID-19 infection using digital proxies of population mobility and mixing. Nat Commun 12, 1501 (2021). https://www.nature.com/articles/s41467-021-21776-2
Big Brother is watching you. However, sometimes he can be helpful. Using digital transactions made on Octopus cards (which are ubiquitously used by the Hong Kong population), the authors describe a framework that integrates digital proxies of human mobility and physical mixing into conventional epidemic models. At the end of the day, real-time estimates of Rt (accurate nowcast and short-term forecast of the epidemic) was obtained in Hong Kong.
9 March
Guy GP Jr., Lee FC, Sunshine G, et al. Association of State-Issued Mask Mandates and Allowing On-Premises Restaurant Dining with County-Level COVID-19 Case and Death Growth Rates — United States, March 1–December 31, 2020. MMWR Morb Mortal Wkly Rep. ePub: 5 March 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7010e3.htm
Mask mandates were associated with statistically significant decreases in county-level daily COVID-19 case and death growth rates within 20 days of implementation. Allowing on-premises restaurant dining was associated with increases in county-level case and death growth rates within 41–80 days after reopening. It will be a while until we can finally go to the restaurant again (does anyone else know how to order a dish?)
4 March
Van Loon W, Hommes F, Theuring S, et al. Renewed absence of SARS-CoV-2 infections in the day care context in Berlin, January 2021. Clinical Infectious Diseases March 2. Full-text: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab199/6155930
The second round of a longitudinal study in 12 randomly selected kindergartens across Berlin including 156 children, 80 staff, and 488 household members of children and staff. According to the authors, repeated absence of SARS-CoV-2 infection four months apart, at weekly community incidences of 38 (first round in September) and 110/100,000, support the initial interpretation that kindergartens are not silent transmission reservoirs.
2 March
Lim T, Delorey M, Bestul N, et al. Changes in SARS CoV-2 Seroprevalence Over Time in Ten Sites in the United States, March – August, 2020. Clin Infect Dis. 2021 Feb 26:ciab185. PubMed: https://pubmed.gov/33639620. Full-text: https://doi.org/10.1093/cid/ciab185
1 March
Mensah AA, Sinnathamby M, Zaidi A, et al. SARS-CoV-2 infections in children following the full re-opening of schools and the impact of national lockdown: prospective, national observational cohort surveillance, July-December 2020, England. J Infection February 24, 2021. https://doi.org/10.1016/j.jinf.2021.02.022
In England, childhood cases closely followed adult infection rates and national lockdown whilst keeping schools open was associated with large declines in SARS-CoV-2 infection rates, first in adults and then in school-aged children. There was a strong correlation in weekly infection rates between adults and all three educational cohorts during periods of both low and high community infection rates. Two messages from this paper: Schools are not the drivers but low community infection rates are required to allow schools to remain open safely.
Hyde Z. Difference in SARS-CoV-2 attack rate between children and adults may reflect bias. Clinical Infectious Diseases 26 February 2021, ciab183, https://doi.org/10.1093/cid/ciab183
In her brief review, Zoë Hyde from Perth, Australia argues that lower secondary attack rates in children compared to adults may reflect lower testing in children and reduced exposure, rather than a genuine difference in biological susceptibility. Additionally, children may shed infectious virus for a shorter period than adults and their antibody response may be less broad, with implications for both polymerase chain reaction and serological testing. After reviewing the data available so far, she thinks it likely that children are more susceptible to SARS-CoV-2 infection than first thought, and they probably play an important role in community transmission.
28 February
Global.health 2021. Link: https://global.health/
This initiave by people from Oxford, Harvard, Northeastern, Boston Children’s Hospital, Georgetown, University of Washington, and Johns Hopkins is meant to be an easy-to-use global data repository and visualization platform that collects anonymized information about individual cases from around the world in one place. The goal: open access to real-time epidemiological anonymized data. See also Maxmen A. Massive Google-funded COVID database will track variants and immunity. Nature. 2021 Feb 24. PubMed: https://pubmed.gov/33627862. Full-text: https://doi.org/10.1038/d41586-021-00490-5
26 February
Lendacki FR, Teran RA, Gretsch S, Fricchione MJ, Kerins JL. COVID-19 Outbreak Among Attendees of an Exercise Facility — Chicago, Illinois, August–September 2020. MMWR Morb Mortal Wkly Rep. ePub: 24 February 2021. DOI: http://dx.doi.org/10.15585/mmwr.mm7009e2
Have you recently met your personal trainer from the local gym? Did he tell you how he disagrees with the lockdown and the closing of the gym, after all they had worked so hard to develop wonderful hygiene management concepts? That all classes would be held at ≤ 25% capacity (i.e., 10–15 persons)? That mask use, temperature checks, symptom screenings would be required on entry (ok, patrons were allowed to remove masks during exercise) and that patrons would bring their own mats and weights and would be stationed ≥ 6 ft apart? Then show him this report. During August 24–September 1, 2020, an exercise facility at Chicago did exactly this. The results: 55 COVID-19 cases were identified among 81 attendees of indoor high-intensity classes. Twenty-two (40%) persons with COVID-19 attended on or after the day symptoms began. Most attendees (76%) wore masks infrequently, including persons with (84%) and without COVID-19 (60%).
Harvey RA, Rassen JA, Kabelac CA, et al. Association of SARS-CoV-2 Seropositive Antibody Test With Risk of Future Infection. JAMA Intern Med February 24, 2021. Full-text: https://doi.org/10.1001/jamainternmed.2021.0366
Seropositivity is associated with protection from infection. In this cohort study of more than 3.2 million US patients with a SARS-CoV-2 antibody test, 0.3% of those indexed with positive test results had evidence of a positive nucleic acid amplification test beyond 90 days after index, compared with 3.0% indexed with negative antibody test results. During the follow-up periods, the ratio (95% CI) of positive PCR results among individuals who had a positive antibody test at index vs those with a negative antibody test at index was 2.85 (95% CI: 2.73-2.97, consistent with prolonged RNA shedding!) at 0 to 30 days, 0.67 at 31 to 60 days, 0.29 at 61 to 90 days, and 0.10 at more than 90 days.
Katz MH. How to Advise Persons Who Are Antibody Positive for SARS-CoV-2 About Future Infection Risk. JAMA Intern Med February 24, 2021. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2776809
In his comment, Mitchell H. Katz still believes that vaccination against SARS-CoV-2 is recommended regardless of antibody status (as nobody knows how long antibody protection due to natural infection will last).
Davido B, Mascitti H, Fortier-Beaulieu M, et al. Blue toes’ following vaccination with the BNT162b2 mRNA COVID-19 vaccine. Journal of Travel Medicine, 23 February 2021, taab024, https://doi.org/10.1093/jtm/taab024
COVID toes-like syndrome linked to COVID-19 vaccine: This interesting case report describes a young Caucasian female (aged 41) who presented with chilblain-like skin changes on her toes that appeared 4 days after the first injection with the Pfizer-BioNTech-162b2 vaccine.
Groves LM, Usagawa L, Elm J, et al. Community Transmission of SARS-CoV-2 at Three Fitness Facilities — Hawaii, June–July 2020. MMWR Morb Mortal Wkly Rep. ePub: 24 February 2021. DOI: http://dx.doi.org/10.15585/mmwr.mm7009e1
Twenty-one COVID-19 cases were linked to an index case in a fitness instructor, who, along with a patient who was also an instructor, taught classes < 1 day, 1 to < 2 days, and ≥ 2 days before symptom onset; aggregate attack rates were 95% (20 of 21), 13% (one of eight), and 0% (zero of 33). Of note, use of masks was not required in the fitness facilities.
24 February
Zimmerman FJ, Anderson NW. Association of the Timing of School Closings and Behavioral Changes With the Evolution of the Coronavirus Disease 2019 Pandemic in the US. JAMA Pediatr February 22, 2021. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2776608
This cross-sectional study used US COVID-19 data (March to May 2020) and anonymized cell phone as well as internet data. The main findings: voluntary behavioral changes, such as reductions in time spent at work, had an association with COVID-19 incidence and mortality that was 3 times stronger than that of school closures. According to Nathaniel W. Anderson and Frederick J. Zimmerman, their findings suggest that less harmful ways of preventing SARS-CoV-2 transmission are available than mandatory school closures (note: this is based on data prior to the occurrence of more transmittable variants).
Gold JA, Gettings JR, Kimball A, et al. Clusters of SARS-CoV-2 Infection Among Elementary School Educators and Students in One School District — Georgia, December 2020–January 2021. MMWR Morb Mortal Wkly Rep. ePub: 22 February 2021. Full-text: http://dx.doi.org/10.15585/mmwr.mm7008e4
Vaccinate and test the teachers! This investigation in a Georgia school district from December 1, 2020 to January 22, 2021, identified nine clusters of COVID-19 cases involving 13 educators and 32 students at six elementary schools. Consistent with findings from international studies, the report found that initial infections among educators played a substantial role in in-school SARS-CoV-2 transmission and subsequent chains of infection to other educators, students, and households, highlighting the importance of preventing infections among educators in particular.
22 February
Paper of the Day
Nelson EJ, McKune SL, Ryan KA, et al. SARS-CoV-2 Positivity on or After 9 Days Among Quarantined Student Contacts of Confirmed Cases. JAMA February 19, 2021. doi:10.1001/jama.2021.2392 https://jamanetwork.com/journals/jama/fullarticle/2776857
Testing at day 9 instead of 14 days of strict quarantine in students: this study found no evidence that an earlier return to school with a negative test result was linked with subsequent symptomatic illness. Among 799 student contacts of confirmed COVID-19 cases with a negative test result on days 9 to 14, only 1 student became symptomatic after returning to school and had a positive SARS-CoV-2 test result on day 14 after an initial negative test result on day 9. The virus from this student was genetically distinct from the virus isolated from the confirmed COVID-19 case to which the student had been exposed.
Brecht I, Peckeu L, Laga M, et al. Reducing contacts to stop SARS-CoV-2 transmission during the second pandemic wave in Brussels, Belgium, August to November 2020. Euro Surveill February 17,. 2021;26(7):pii=2100065. https://doi.org/10.2807/1560-7917.ES.2021.26.7.2100065
This study shows how stringent physical distancing measures (a limit to three close contacts per person, a curfew, closure of bars and recommended teleworking) that were introduced 1 month after a persistent increase in Rt, sufficiently controlled transmission in Belgium, even with high case numbers and without closing schools or full lockdown (remember, this was prior to the occurrence of B.1.1.7).
20 February
Mwananyanda L, Gill CJ, MacLeod W, et al. Covid-19 deaths in Africa: prospective systematic postmortem surveillance study. BMJ. 2021 Feb 17;372:n334. PubMed: https://pubmed.gov/33597166. Full-text: https://doi.org/10.1136/bmj.n334
Do we vastly underestimate the impact of COVID-19 in Africa? Maybe. In this study of all deceased people of all ages at a University Hospital in Lusaka, Zambia, 70/364 (19,2%) were PCR positive. Most deaths in people with COVID-19 (51/70; 73%) occurred in the community; none had been tested for SARS-CoV-2 before death.
18 February
Emanuel EJ, Bright R, Gounder C. A Dismal Spring Awaits Unless We Slow the Spread of Covid-19. The New York Times 2021, published 17 February. Full-text: https://www.nytimes.com/2021/02/17/opinion/covid-19-precautions.html
How soon life returns to normal depends on what we do now.
17 February
Phillips N. The coronavirus is here to stay — here’s what that means. Nature 2021, published 16 February. Full-text: https://www.nature.com/articles/d41586-021-00396-2
A Nature survey shows many scientists expect the virus that causes COVID-19 to become endemic, but it could pose less danger over time.
16 February
Shallcross L, Burke D, Abbott O. Factors associated with SARS-CoV-2 infection and outbreaks in long-term care facilities in England: a national cross-sectional survey. Lancet Health Longevity 2021, published 11 February. Full-text: https://doi.org/10.1016/S2666-7568(20)30065-9
Laura Shallcross et al. found that half of long-term care facilities (LTCFs) in England had no cases of SARS-CoV-2 infection in the first wave of the pandemic. Reduced transmission from staff is associated with (there is a lesson here!)
- adequate sick pay,
- minimal use of agency staff,
- an increased staff-to-bed ratio, and
- staff cohorting with either infected or uninfected residents.
Increased transmission from residents is associated with an increased number of new admissions to the facility and poor compliance with isolation procedures.
21 Febuary
Tian L, Li X, Qi F et al. Harnessing peak transmission around symptom onset for non-pharmaceutical intervention and containment of the COVID-19 pandemic. Nat Commun February 19, 2021. https://www.nature.com/articles/s41467-021-21385-z
Epidemiological modeling study, focusing on transmission around symptom onset by both pre-symptomatic and symptomatic viral carriers.
15 February
Hay JA, Kennedy-Shaffer L, Kanjilal S, et al. Estimating epidemiologic dynamics from cross-sectional viral load distributions. MedRxiv 2021, posted 13 February. Full-text: https://doi.org/10.1101/2020.10.08.20204222
Cycle threshold (Ct) values from even limited numbers of random samples might provide estimates of an epidemic’s trajectory. Michael Mina, Marc Lipsitch, James Hay and colleagues applied their methods to Ct values from surveillance conducted during the SARS-CoV-2 pandemic in a variety of settings. A new approach for real-time estimates of epidemic trajectories for outbreak management and response?
Helix 202102. The Helix® COVID-19 Surveillance Dashboard. Helix 2021; website: https://www.helix.com/pages/helix-covid-19-surveillance-dashboard
The B.1.1.7 strain is doubling every 10 days in the US. Should it be the last obstacle to achieving containment of SARS-CoV-2 in the country? Wait a few weeks before eliminating effective mitigation measures such as mask mandates and bans on gatherings.
Alpert T, Lasek-Nesselquist E, Brito AF, et al. Early introductions and community transmission of SARS-CoV-2 variant B.1.1.7 in the United States. medRxiv 2021, posted 12 February. Full-text: https://doi.org/10.1101/2021.02.10.21251540
Nathan D. Grubaugh, Tara Alpert and colleagues highlight the primary ports of entry for B.1.1.7 in the US. New York is likely one of the key hubs for introductions and domestic spread. The authors also provide evidence for increased community transmission in several states.
14 February
Jahn K, Dreifuss D, Topolsky I, et al. Detection of SARS-CoV-2 variants in Switzerland by genomic analysis of wastewater samples. medRxiv 2021, posted 9 February. Full-text: https://doi.org/10.1101/2021.01.08.21249379
Katharina Jahn et al. found evidence for the presence of several mutations that define B117 and B1351 in a sample from a Swiss ski resort from 9-21 December, two weeks before its first verification in a patient sample from Switzerland. The authors conclude that sequencing SARS-CoV-2 in community wastewater samples may help detect and monitor the circulation of diverse lineages.
Ward H, Atchison C, Whitaker M, et al. SARS-CoV-2 antibody prevalence in England following the first peak of the pandemic. Nat Commun 12, 905 (2021). Full-text: https://doi.org/10.1038/s41467-021-21237-w
According to this study by Paul Elliott, Helen Ward and colleagues, an estimated 3,4 million people had developed antibodies to SARS-CoV-2 by mid-July 2020. Prevalence was two- to three-fold higher among health and care workers compared with non-essential workers, and in people of Black or South Asian than white ethnicity. The authors conclude that higher hospitalization and mortality from COVID-19 in minority ethnic groups may reflect higher rates of infection rather than differential experience of disease or care.
12 February
Carrat F, Figoni J, Henny J, et al. Evidence of early circulation of SARS-CoV-2 in France: findings from the population-based “CONSTANCES” cohort. Eur J Epidemiol (2021). Full-text: https://doi.org/10.1007/s10654-020-00716-2
Using serum samples routinely collected in 9144 adults from a French general population-based cohort, Fabrice Carrat et al. identified 13 participants with a positive anti-SARS-CoV-2 IgG test between November 2019 and January 2020. The results were confirmed by neutralizing antibodies testing. Investigations in 11 of these participants revealed experience of symptoms possibly related to a SARS-CoV-2 infection or situations of risk of potential SARS-CoV-2 exposure. This report suggests early circulation of SARS-CoV-2 in Europe.
11 February
Grubaugh ND, Hodcroft EB, Fauber JR, Phelan AL, Cevik M. Public health actions to control new SARS-CoV-2 variants. Cell 2021, published 29 January. Full-text: https://www.cell.com/cell/fulltext/S0092-8674(21)00087-8
The emergence of more transmissible variants will exacerbate the pandemic and reduce the efficacy of some vaccines. Nathan D. Grubaugh and colleagues provide public health guidance for increased surveillance and measures to reduce community transmission. Much of this article uses the B117 variant as an example, but similar principles can be applied to other SARS-CoV-2 variants, including B1351 and P1.
Chen YH, Glymour M, Riley A, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through October 2020. MedRxiv 2021, posted 22 January. Full-text: https://www.medrxiv.org/content/10.1101/2021.01.21.21250266v1?s=09
Risk ratios for mortality comparing pandemic time to non-pandemic time were highest among cooks (RR=1.60), packaging and filling machine operators (RR=1.59), miscellaneous agricultural workers (RR=1.55), bakers (RR=1.50), and construction laborers (RR=1.49).
10 February
Zeller M, Gangavarapu K, Anderson C, et al. Emergence of an early SARS-CoV-2 epidemic in the United States. medRxiv 2021, posted 8 February. Full-text: https://www.medrxiv.org/content/10.1101/2021.02.05.21251235v1
Superspreading during large-scale events plays a key role in the COVID-19 pandemic. The city of New Orleans, US, experienced one of the earliest and fastest accelerating outbreaks, coinciding with the annual Mardi Gras festival, which went ahead without precautions. Here, Kristian G. Andersen, Mark Zeller and colleagues sequence SARS-CoV-2 genomes during the first wave of the COVID-19 epidemic in Louisiana. They show that the Mardi Gras festival (25 Feb 2020 and the weeks leading up to it) dramatically accelerated transmission, eventually leading to secondary localized COVID-19 epidemics throughout the Southern US.
Staub K, Jüni P, Urner M, et al. Public Health Interventions, Epidemic Growth, and Regional Variation of the 1918 Influenza Pandemic Outbreak in a Swiss Canton and Its Greater Regions. Ann Intern Med. 2021 Feb 9. PubMed: https://pubmed.gov/33556268. Full-text: https://doi.org/10.7326/M20-6231
Strikingly similar patterns were found in the management of the COVID-19 outbreak in Switzerland, with a considerably higher amplitude and prolonged duration of the second wave and much higher associated rates of hospitalization and mortality. During the second wave in autumn, cantonal authorities reacted hesitantly and initially delegated the responsibility to enact public health measures to the municipalities. This hesitant attitude was largely due to concerns about the economic effect of public health interventions experienced during the first wave and the associated political pressure. Read also the comment by Mooney G. The Dangers of Ignoring History Lessons During a Pandemic. Ann Intern Med. 2021 Feb 9. PubMed: https://pubmed.gov/33556270. Full-text: https://doi.org/10.7326/M21-0449
9 February
Davies N, Abbott S, Barnard C, et al. Estimated transmissibility and severity of novel SARS-CoV-2 Variant of Concern 202012/01 in England. CMMID Repository 2021, updated 6 February. Full-text: https://cmmid.github.io/topics/covid19/uk-novel-variant.html?s=09
The authors estimate that B117 is 43–82% (range of 95% credible intervals 38–106%) more transmissible than pre-existing variants of SARS-CoV-2. We find that without stringent control measures, COVID-19 hospitalizations and deaths are projected to reach higher levels in 2021 than were observed in 2020. Control measures of a similar stringency to the national lockdown implemented in England in November 2020 would be unlikely to reduce the effective reproduction number Rt to less than 1, unless primary schools, secondary schools, and universities are also closed.
8 February
Mohanan M, Malani A, Krishnan K, Acharya A. Prevalence of SARS-CoV-2 in Karnataka, India. JAMA. 2021 Feb 4. PubMed: https://pubmed.gov/33538774. Full-text: https://doi.org/10.1001/jama.2021.0332
The adjusted seroprevalence of SARS-CoV-2 across Karnataka, India, was 46,7%, suggesting approximately 31,5 million residents were infected, far greater than the 327.076 cases reported by August 29, 2020.
Gaudart J, Landier J, Huiart L, et al. Factors associated with the spatial heterogeneity of the first wave of COVID-19 in France: a nationwide geo-epidemiological study. Lancet Public Health 2021, published 5 February. Full-text: https://doi.org/10.1016/S2468-2667(21)00006-2
From March 19 to May 11, 2020, hospitals in metropolitan France notified a total of 100.988 COVID-19 cases, including 16.597 people who were admitted to intensive care and 17.062 deaths. Mortality and case fatality rates were higher in regions with older populations. Jean Gaudart et al. found no association between climate and in-hospital COVID-19 incidence, or between economic indicators and in-hospital COVID-19 incidence or mortality rates.
Roederer T, Mollo B, Vincent C, et al. Seroprevalence and risk factors of exposure to COVID-19 in homeless people in Paris, France: a cross-sectional study. Lancet Public Health 2021, published 5 February. Full-text: https://doi.org/10.1016/S2468-2667(21)00001-3
During the COVID-19 lockdown period from March 17 to May 11, 2020, French authorities in Paris and its suburbs relocated people experiencing recurrent homelessness to emergency shelters, hotels, and large venues. In this study by Thomas Roederer et al., more than half of surveyed individuals (426 of 818, 52%) tested positive by any serological test. Seroprevalence was highest among those living in workers’ residences (88,7%), followed by emergency shelters (50,5%), and food distribution sites (27,8%). More than two thirds of COVID-19 seropositive individuals (68%) did not report any symptoms during the recall period. Living in crowded conditions was the strongest factor associated with exposure level. This study underscores the importance of providing safe, uncrowded accommodation, alongside adequate testing and public health information.
7 February
Kamps BS. Variants – 6 February update. COVID Reference 2021, published 6 February. Full-text: https://covidreference.com/variants | See also the Comparison document with new additions between 31 January and 6 February: http://www.bsk1.com/CR_Variants_Update.html
In many countries, the more transmissible SARS-CoV-2 variants B117, B1351 and P1 are currently replacing previously dominating lineages. B117, B1351 and P1 are already dominant in England (B117), South Africa (B1351) and Amazonia (P1). They also account for 50% or more of new infections in Ireland, Portugal and Israel (B117). Over the coming weeks, B117 will spread through most countries in continental Europe and the US.
6 February
Quammen D. How viruses shape our world – COVID-19 is a reminder of their destructive power, but they’re crucial to humans’ development and survival. National Geographic 2021, published 14 January. Full-text: https://www.nationalgeographic.com/magazine/2021/02/viruses-can-cause-great-harm-but-we-could-not-live-without-them-feature/
“Although feared as agents of disease, viruses also work wonders, shaping evolution from the very beginning. About 8 percent of our DNA comes from viruses that infected our long-ago ancestors and patched viral genes into their genomes. Some of these genes now play crucial roles in the early stages of the developing embryo and the placenta that surrounds this 13-week-old fetus.”
Bruckner TA, Parker DM, Bartell SM, et al. Estimated seroprevalence of SARS-CoV-2 antibodies among adults in Orange County, California. Sci Rep 11, 3081 (2021). Full-text: https://doi.org/10.1038/s41598-021-82662-x
In Orange County, a densely populated and diverse county in southern California, the SARS-CoV-2 seroprevalence in July and August 2020 may have been approximately 12 percent, seven-fold greater than the reported cases.
5 February
Monod M, Blenkinsop A, Xi X, et al. Age groups that sustain resurging COVID-19 epidemics in the United States. Science. 2021 Feb 2:eabe8372. PubMed: https://pubmed.gov/33531384. Full-text: https://doi.org/10.1126/science.abe8372
As of October 2020, individuals aged 20-49 are the only age groups sustaining resurgent SARS-CoV-2 transmission with reproduction numbers well above one, and at least 65 / 100 COVID-19 infections originate from individuals aged 20-49 in the US.
4 February
Kissane E, Madrigal A. It’s Time: The COVID Tracking Project Will Soon Come to an End. The COVID Tracking Project 2021, published 1 February. Full-text: https://covidtracking.com/analysis-updates/covid-tracking-project-end-march-7
After a year of collecting, analyzing, and interpreting COVID-19 data for the United States, we’re ending our data compilation work in early March. When should COVID Reference shut down its activity?
3 February
Public Health England 20210115. Investigation of novel SARS-COV-2 variant: Variant of Concern 202012/01 – Technical briefing 5. UK Government 2021, updated 2 February; accessed 2 February 2021. Full-text: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/957504/Variant_of_Concern_VOC_202012_01_Technical_Briefing_5_England.pdf
The key messages:
- The spike protein mutation E484K has been detected in 11 B117 sequences (page 17). Preliminary information suggests more than one acquisition event.
- Estimated attack rates for cases with SGTF are 25 – 40% higher than estimated attack rates for cases with S gene detection results and no SGTF for most regions and age groups, excepting groups with few records such as the 80+ age group (page 17).
29 January
Sabino EC, Buss LF, Carvalho MPS, et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet 2021, published 27 January. Full-text: https://doi.org/10.1016/S0140-6736(21)00183-5
This is not a retraction of the pre-print paper posted on 21 September or of the 8 December Science article below. But in view of the dramatic second wave of the COVID-19 pandemic in Manaus (if you read Spanish, read 111, 222, 333, 444, 555, 666, 777), it is difficult to believe that there has ever been a “75% attack rate of SARS-CoV-2 in the Brazilian Amazon”. [Buss LF, Prete Jr A, Abrahim CMM, et al. Three-quarters attack rate of SARS-CoV-2 in the Brazilian Amazon during a largely unmitigated epidemic. Science 2020, published 8 December. Full-text: https://doi.org/10.1126/science.abe9728]. The future will tell.
Lopreite M, Panzarasa P, Puliga M, et al. Early warnings of COVID-19 outbreaks across Europe from social media. Sci Rep 11, 2147 (2021). https://doi.org/10.1038/s41598-021-81333-1
The authors analyzed data from Twitter to uncover early-warning signals of the coming COVID-19 pandemic in Europe. Whistleblowing came primarily from the geographical regions that eventually turned out to be the key breeding grounds for infections. So, start setting up an integrated digital surveillance system in which social media will geo-localize chains of contagion.
28 January
Borges V, Sousa C, Menezes L, et al. Tracking SARS-CoV-2 VOC 202012/01 (lineage B.1.1.7) dissemination in Portugal: insights from nationwide RT-PCR Spike gene drop out data. Virological.org 2021, published 19 January. Full-text: https://virological.org/t/tracking-sars-cov-2-voc-202012-01-lineage-b-1-1-7-dissemination-in-portugal-insights-from-nationwide-rt-pcr-spike-gene-drop-out-data/600
Portugal is facing a highly dynamic epidemic situation. Here, João P Gomes, Vítor Borges and colleagues show that the B.1.1.7 variant represented 5,8% of all positive cases detected since week 49 of 2020 and 13,3% by the end of week 2, 2021. The authors anticipate that B.1.1.7 might reach up to 60% of positive cases by early February 2021. Robust public health measures on the horizon.
24 January
Quilty BJ, Clifford S, Hellewell J, et al. Quarantine and testing strategies in contact tracing for SARS-CoV-2: a modelling study. Lancet Public Health January 20, 2021. DOI:https://doi.org/10.1016/S2468-2667(20)30308-X
The main results of this modelling study: quarantine until a PCR or lateral flow antigen test on day 7 after exposure (with early release if negative) might avert as much transmission as a 14-day quarantine period. Additionally, daily repeated lateral flow antigen testing of traced contacts for 5 days, with isolation only after a positive test, might allow for the quarantine requirement to be removed with a small increase in transmission risk, which could itself be offset by increased participation and adherence to isolation. (A visual would be great here)
22 January
Somekh I, Shohat T, Boker LK, Simões EAF, Somekh E. Reopening Schools and the Dynamics of SARS-CoV-2 Infections in Israel: A Nationwide Study. Clin Infect Dis. 2021 Jan 18:ciab035. PubMed: https://pubmed.gov/33460434. Full-text: https://doi.org/10.1093/cid/ciab035
This analysis does not support that school reopening played a major role in the resurgence of the COVID-19 curve (between March and July 2020) in Israel. Easing restrictions on large scale gatherings was the major influence on this resurgence.
Lewis D. What new COVID variants mean for schools is not yet clear. Nature 21 January 2021, https://www.nature.com/articles/d41586-021-00139-3
Read the title out loud. Dyani Lewis summarizes current knowledge. Children are no more susceptible to these lineages than adults are — and closing schools on the basis of incomplete information could have serious repercussions. The debate continues.
Priesemann V, Balling R, Brinkmann MM, et al. An action plan for pan-European defence against new SARS-CoV-2 variants. Lancet January 21, 2021. Full-text: https://doi.org/10.1016/S0140-6736(21)00150-1
According to Viola Priesemann and colleagues, core measures to prevent the spread of SARS-CoV-2 in Europe are:
- Achieve and maintain low case numbers with a clear prevention strategy
- Monitor the spread of the virus and of individual variants
- Stop the virus before it crosses borders
- Protect the vulnerable
- Increase the pace of administration of vaccines
The core principles of action are to avoid importing new variants, to prevent their spread, and to improve molecular surveillance. The earlier and more effectively countries act, the earlier the restrictions can be relaxed. All types of measures ought to be coordinated and synchronized across Europe. Every additional reduction of contagion counts, as it reduces the necessary duration of strict measures more than 1:1.
Bartsch M, Bohr F, von Bredow R, et al. Can We Stop a Super Coronavirus? Der Spiegel 2021, published 19 January. Full-text: https://www.spiegel.de/international/world/can-germany-stop-the-new-supervirus-a-e9ffc207-0015-4330-8361-b306f6053e15
The new variants of the coronavirus are even more dangerous than those known so far. Researchers and politicians fear a sharp increase in the number of infections, with dramatic consequences like those seen in Britain. Can Germany still stop the new killers?
21 January
Gouvea-Reis FA, Oliveira PD, et al. COVID-19 outbreak in a large penitentiary complex, April–June 2020, Brazil. Emerg Infect Dis, March 2021. Full-text: https://doi.org/10.3201/eid2703.204079
Faster viral spread in overcrowded settings: the mean serial interval during this large SARS-CoV-2 outbreak at a Brazilian prison was only 2,51 days. Between April 1 and June 12, there were 1057 reported cases: 859 (81,3%) in inmates, 180 (17,1%) in prison guards, 9 (0,8%) in contracted staff, and 9 (0,8%) in health professionals. Nine patients were hospitalized, and 3 deaths were reported: 1 prison guard and 2 inmates.
20 January
Mervosh S, Baker M, Mazzei P, Walker M. One Year, 400,000 Coronavirus Deaths: How the U.S. Guaranteed Its Own Failure. The New York Times 2021, published 17 January. Full-text: https://www.nytimes.com/2021/01/17/us/covid-deaths-2020.html
After the White House declined to pursue a unified national COVID strategy, governors faced off against lobbyists, health experts and a restless public consumed by misinformation.
19 January
Oliva C, Di Maddaloni F, Marcellusi A, Favato G. Cross-regional variations of Covid-19 mortality in Italy: an ecological study. J Public Health 2021, published 18 January. Full-text: https://doi.org/10.1093/pubmed/fdaa248
Four independent variables best explained the cross-regional differences in the number of deaths attributed to COVID-19: the force of infection, population density, number of elderly living in assisted facilities and the standard rate of diabetes.
Nørgaard SK, Vestergaard LS, Nielsen J, et al. Real-time monitoring shows substantial excess all-cause mortality during second wave of COVID-19 in Europe, October to December 2020. Euro Surveill. 2021 Jan;26(2). PubMed: https://pubmed.gov/33446304. Full-text: https://doi.org/10.2807/1560-7917.ES.2021.26.1.2002023
No comment.
18 January
Faria NR, Claro IM, Candido D, et al. Genomic characterisation of an emergent SARS-CoV-2 lineage in Manaus: preliminary findings. Virological.org 2021, posted 12 January. Full-text: https://virological.org/t/genomic-characterisation-of-an-emergent-sars-cov-2-lineage-in-manaus-preliminary-findings/586
A new variant (P.1, descendent of B.1.1.28) was circulating in December 2020 in Manaus, Amazonas state, and was identified in 42% (13 out of 31) of RT-PCR positive samples collected between 15 and 23 December. These findings indicate local transmission and possibly recent increase in the frequency of a new lineage from the Amazon region. P.1 contains several mutations of known biological importance such as E484K, K417T, and N501Y. Read also Kupferschmidt K. New coronavirus variants could cause more reinfections, require updated vaccines. Nature 2021, published 15 January. Full-text: https://www.sciencemag.org/news/2021/01/new-coronavirus-variants-could-cause-more-reinfections-require-updated-vaccines
17 January
Galloway SE, Paul P, MacCannell DR, et al. Emergence of SARS-CoV-2 B.1.1.7 Lineage — United States, December 29, 2020–January 12, 2021. MMWR Morb Mortal Wkly Rep. ePub: 15 January 2021. Full-text: http://dx.doi.org/10.15585/mmwr.mm7003e2
B117, a more highly transmissible variant of SARS-CoV-2 has been detected in 10 US states. CDC recommends universal and increased compliance with mitigation strategies, including distancing and masking, and ramping up the vaccination campaign. The following figure shows how a more infectious virus could lead to many more deaths. Simplified, hypothetical scenario showing the number of new deaths every six days from three different virus strains, assuming each strain started from 10.000 infections. Source: Adam Kucharski, London School of Hygiene and Tropical Medicine.
Sridhar D, Gurdasani D. Herd immunity by infection is not an option. Science. 2021 Jan 15;371(6526):230-231. PubMed: https://pubmed.gov/33446540. Full-text: https://doi.org/10.1126/science.abf7921
A must-read by Devi Sridhar and Deepti Gurdasani. Do you remember ‘herd immunity in Brazil’? On 26 September 2020 we presented a medRxiv post by Buss et al. with a title suggesting that herd immunity might have been reached in Brazil’s Amazon region around Manaus. [Buss LF, Prete Jr CA, Abrahim CMM, et al. COVID-19 herd immunity in the Brazilian Amazon. medRxiv 2020, posted 21 September. Full-text: https://doi.org/10.1101/2020.09.16.20194787.] In the meantime, the title of the paper was changed to Three-quarters attack rate of SARS-CoV-2 in the Brazilian Amazon during a largely unmitigated epidemic (13 December) and there is no herd immunity anymore in Manaus (The Guardian, 14 January).
Ranzani TO, Bastos LSL, Gelli JBM, et al. Characterisation of the first 250 000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med 2021, published 15 January. Full-text: https://doi.org/10.1016/S2213-2600(20)30560-9
In-hospital mortality among patients younger than 60 years was 31% (4204 of 13.468) in the Brazilian Northeast versus 15% (1694 of 11.196) in the South in this retrospective analysis by Fernando Bozza, Otavio Ranzani and colleagues. In their study, the authors included 232.036 patients admitted to hospital in Brazil between 16 February and 15 August 2020. In-hospital mortality was 38% (87.515 of 232.036 patients) overall, 59% (47.002 of 79.687) among patients admitted to the ICU, and 80% (36.046 of 45.205) among those who were mechanically ventilated.
15 January
Ledford H. COVID reinfections are unusual — but could still help the virus to spread. Nature 2021, published 14 January. Full-text: https://www.nature.com/articles/d41586-021-00071-6
A large study of UK healthcare workers suggests that most people are immune for months after catching COVID-19 for the first time.
Ashby B, Best A. Herd immunity. Curr Biol 2021, published 12 January. Full-text: https://doi.org/10.1016/j.cub.2021.01.006
If you want to do some math, read this short paper and revise a concept neither Boris Johnson (how could he!) nor his advisers really understood. In short: as immunity accumulates in a population — naturally during the course of an epidemic or through vaccination — the spread of infectious disease is limited by the depletion of susceptible hosts. In this primer, Ben Ashby and Alex Best discuss the concept of herd immunity from first principles, clarify common misconceptions, and consider the implications for disease control.
14 January
Vang KE, Krow-Lucal ER, James AE, et al. Participation in Fraternity and Sorority Activities and the Spread of COVID-19 Among Residential University Communities – Arkansas, August 21-September 5, 2020. MMWR Morb Mortal Wkly Rep. 2021 Jan 8;70(1):20-23. PubMed: https://pubmed.gov/33411698. Full-text: https://doi.org/10.15585/mmwr.mm7001a5
In the US, the start of the 2020–21 academic year was sometimes the beginning of local epidemics. Kristyn Vang et al. describe SARS-CoV-2 transmission by on- and off-campus congregate living settings and activities. Their analysis indicates that 91% of gatherings were associated with fraternity or sorority activities. Interestingly, at one university, women accounted for 70% of COVID-19 cases although they constituted only 54% of the university’s student body. Among linked gatherings, women accounted for 86% of cases. The authors speculate about possible explanations (involvement in gender-specific activities? sorority rush week?).
13 January
Bagchi S, Mak J, Li Q, et al. Rates of COVID-19 Among Residents and Staff Members in Nursing Homes — United States, May 25–November 22, 2020. MMWR Morb Mortal Wkly Rep. ePub: 8 January 2021. DOI: http://dx.doi.org/10.15585/mmwr.mm7002e2
Increases in community rates might be associated with increases in nursing home COVID-19 incidence, and nursing home mitigation strategies need to include a comprehensive plan to monitor local SARS-CoV-2 transmission and minimize high-risk exposures within facilities.
11 January
Charron N, Lapuente V, Rodriguez-Pose A. Uncooperative Society, Uncooperative Politics or Both? How Trust, Polarization and Populism Explain Excess Mortality for COVID-19 across European regions. The Quality of Government (QoG) Institute 2020 (December). Full-text: https://gupea.ub.gu.se/handle/2077/67189
Why have some places performed better than others in the fight against COVID-19? The authors found that societal polarization played a significant role. When the divide in political trust between supporters and opponents of incumbent governments within societies is high, the authors observe consistently higher COVID-19-related excess mortality deaths during the first wave of the pandemic. They also find that regions with a political elite less supportive of European integration are regions where excess deaths have been significantly higher. Vive l’Europe!
9 January
Leung K, Shum MH, Leung GM, Lam TT, Wu JT. Early transmissibility assessment of the N501Y mutant strains of SARS-CoV-2 in the United Kingdom, October to November 2020. Euro Surveill. 2021 Jan;26(1). PubMed: https://pubmed.gov/33413740. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.26.1.2002106
Two new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) lineages carrying the amino acid substitution N501Y in the receptor-binding domain (RBD) of the spike protein have spread rapidly in the United Kingdom (UK) during late autumn 2020. Tommy Lam, Joseph Wu, Kathy Leung and colleagues explain that 501Y Variant 2 (also named B.1.1.7, 20B/501Y.V1 and VOC-202012/01) is estimated to present an R0 1.75 times higher than 501N, meaning it is 75% more transmissible compared with the 501N strain.
du Plessis L, McCrone JT, Zarebski AE, et al. Establishment and lineage dynamics of the SARS-CoV-2 epidemic in the UK. Science 2021, published 8 January. Full-text: https://doi.org/10.1126/science.abf2946
In early 2020, pre-lockdown, high travel volumes and few restrictions on international arrivals led to the establishment and co-circulation of >1000 identifiable UK transmission lineages, jointly contributing to accelerated epidemic growth that quickly exceeded national contact tracing capacity. The authors reveal the fine-scale genetic lineage structure of this early epidemic through analysis of 50,887 SARS-CoV-2 genomes, including 26,181 from the UK sampled throughout the country’s first wave of infection.
Yang DD, Ouldali N, Gajdos V, et al. Common pediatric respiratory infectious diseases may serve as an early predictor for SARS-CoV-2 new wave of infections. Clin Infect Dis. 2020 Sep 7:ciaa1359. PubMed: https://pubmed.gov/32894752. Full-text: https://doi.org/10.1093/cid/ciaa1359
Lockdowns lead to a decrease in the common cold, bronchiolitis, acute otitis media, and acute gastroenteritis (AGE) in children. Having found that, François Angoulvant, David Yang and colleagues were curious to know what would happen after the end of the lockdown and analyzed a total of 908.887 pediatric emergency visits from 6 academic hospitals over the last three years. As expected, two weeks after the lockdown, observed values reached expected values for the common cold, bronchiolitis, and acute asthma exacerbation. There was one surprise, though: there was no increase in AGE after the end of lockdown. The authors suggest continued regular handwashing and the use of alcohol-based sanitizers as an explanation for this finding. They conclude that the positive lessons learned from SARS-CoV-2, especially handwashing and social distancing, should not be forgotten after the pandemic.
8 January
Kirby T. New variant of SARS-CoV-2 in UK causes surge of COVID-19. Lancet Respir Med 2021, published 5 January. Full-text: https://doi.org/10.1016/S2213-2600(21)00005-9
The UK remains one of the most badly affected countries. As of 6 January 2021, it had recorded more than 2,8 million cases of SARS-CoV-2 infection and almost 80.000 deaths. Driven by the new variant’s increased infectiousness, the UK has recently reported more than 60.000 cases a day, and there are fears that the pandemic may get very much worse before it gets better. The only hope now is that deaths and hospitalizations will plummet as the number of elderly and vulnerable people receiving a vaccine sharply increases in the coming weeks.
7 January
Veldhoen M, Simas JP. Endemic SARS-CoV-2 will maintain post-pandemic immunity. Nat Rev Immunol (2021). Full-text: https://doi.org/10.1038/s41577-020-00493-9
Marc Veldhoen and J. Pedro Simas predict that the maintenance of population immunity will not depend on continued vaccinations but on the endemic presence of SARS-CoV-2. The authors offer an intriguing long-term perspective: “Endemic SARS-CoV-2 will ensure maintenance of seroprevalence and mucosal immunity in the population, which will increase over time in new generations. As such, most infected individuals will ultimately endure a largely asymptomatic or mild course of disease, although similarly to the other common cold HCoVs, SARS-CoV-2 may cause fatalities in extremely vulnerable elderly or immunocompromised individuals.”
Ives AR, Bozzuto C. Estimating and explaining the spread of COVID-19 at the county level in the USA. Commun Biol 4, 60 (2021). Full-text: https://doi.org/10.1038/s42003-020-01609-6
Different states and counties in the USA, and different countries in the world, have experienced COVID-19 epidemics differently. Here, Anthony Ives and Claudio Bozzuto put numbers on these differences in the USA. The authors show that most of the high inter-county variance is explained by four factors (R2 = 0.70): the timing of the outbreak, population size, the population density, and spatial location. Their recommendation for the future: design public health interventions at the county level.
4 January
Maeda JM, NkengasongJN. The puzzle of the COVID-19 pandemic in Africa. Science 2021, published 1 January. Full-text: https://doi.org/10.1126/science.abf8832
As of 22 November 2020, the continent of Africa, comprising 1,3 billion people, had recorded two million cases of COVID-19 and 50.000 deaths, representing ∼ 3.6% of total global cases. Why? Justin Maeda and John Nkengasong comment on a paper we previously presented on 13 November: Uyoga S, Adetifa IMO, Karanja HK, et al. Seroprevalence of anti–SARS-CoV-2 IgG antibodies in Kenyan blood donors. Science 2020, published 11 November. Full-text: https://doi.org/10.1126/science.abe1916 | In April-June 2020, the crude prevalence of anti–SARS-CoV-2 IgG among blood donors in Kenya was 5.6% (174/3098). It was highest in urban counties, Mombasa (8.0%), Nairobi (7.3%) and Kisumu (5.5%). Of note, Kenya had reported only 341 deaths by the end of that period. The authors conclude that the sharp contrast between the reported COVID-19 cases and deaths suggests that the disease might be attenuated in Africa.
3 January
Duca LM, Xu L,Price SF, McLean C. COVID-19 Stats: COVID-19 Incidence, by Age Group — United States, March 1–November 14, 2020. MMWR Morb Mortal Wkly Rep 2021;69:1664. http://dx.doi.org/10.15585/mmwr.mm695152a8
1 January
Public Health England. Investigation of novel SARS-COV-2 variant: Variant of Concern 202012/01. UK Government 2020, updated 28 December. Full-text: https://www.gov.uk/government/publications/investigation-of-novel-sars-cov-2-variant-variant-of-concern-20201201
The investigation into the new SARS-CoV-2 variant which has spread rapidly within the UK. The authors found that the new variant substantially increases transmissibility.
26 December
Millán-Guerrero RO, Caballero-Hoyos R, Monárrez-Espino J. Poverty and survival from COVID-19 in Mexico. J Pub Health 2020, published 24 December. Full-text: https://doi.org/10.1093/pubmed/fdaa228
Individuals living in municipalities with extreme poverty had a 9% higher risk of dying than those living in municipalities classified as not poor. This is the result of a retrospective Mexican cohort study of nearly 250.000 COVID-19 patients. Mortality was 12,3% reaching 59,3% in patients with ≥ 1 co-morbidities. Combating extreme poverty needs to be a central preventive strategy.
Niu J, Rodriguez JA, Sareli C, et al. COVID-19 infection among first responders in Broward County, Florida, March–April 2020. Journal of Public Health 2020, published 24 December. Full-text: https://doi.org/10.1093/pubmed/fdaa231
Due to job-related exposures, first responders (FRs) are at a higher risk of SARS-CoV-2 infection than the general population. Here, Paula Eckardt, Jianli Niu and colleagues from Memorial Healthcare System, Hollywood, screened a total of 3375 FRs between March and April 2020. Overall, 289 (8,6%) were positive, with the highest rates among those aged 25-49 years. Of those testing positive, 235 (81,3%) were asymptomatic.
25 December
Wurtzer S, Marechal V, Mouchel JM, et al. Evaluation of lockdown effect on SARS-CoV-2 dynamics through viral genome quantification in waste water, Greater Paris, France, 5 March to 23 April 2020. Euro Surveill. 2020 Dec;25(50). PubMed: https://pubmed.gov/33334397. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.50.2000776
Management of epidemics requires careful monitoring of the infected population because special measures such as lockdowns rely on this kind of information. Here, Laurent Moulin and colleagues from Eau de Paris report the analysis of raw waste water (WW) collected at the inlets of waste water treatment plants (WWTPs). They demonstrate that a quantitative detection of SARS-CoV-2 in WW reflects the circulation of the virus in the human population in Greater Paris.
24 December
da Silva Filipe A, Shepherd JG, Williams T, et al. Genomic epidemiology reveals multiple introductions of SARS-CoV-2 from mainland Europe into Scotland. Nat Microbiol 6, 112–122 (2021). Full-text: https://doi.org/10.1038/s41564-020-00838-z
During the first month of the SARS-CoV-2 outbreak in Scotland, 2641 cases of COVID-19 led to 1832 hospital admissions, 207 intensive care admissions and 126 deaths. Here, Emma Thomson, Ana da Silva Filipe and colleagues sequenced 1314 SARS-CoV-2 viral genomes and show that SARS-CoV-2 was introduced to Scotland on at least 283 occasions during February and March 2020. Early introductions of SARS-CoV-2 originated from mainland Europe (the majority from Italy and Spain). The authors identified subsequent early outbreaks in the community, within healthcare facilities and at an international conference. The authors conclude that the risk of multiple reintroduction events in future waves of infection remains high in the absence of population immunity.
23 December
Pullano G, Di Domenico L, Sabbatini CE, et al. Underdetection of COVID-19 cases in France threatens epidemic control. Nature 2020, published 21 December. Full-text: https://doi.org/10.1038/s41586-020-03095-6
In the first 7 weeks following the end of the French lockdown on 11 May 2020, 90.000 cases (9 out of 10 cases) may not have been ascertained by the national surveillance system. Vittoria Colizza, Giulia Pullano and colleagues suggest that more aggressive, targeted and efficient testing is required to act as a pandemic-fighting tool. They warn that a coherent testing strategy will be again of critical value to avoid a third SARS-CoV-2 wave in the coming months.
See also the NEWS AND VIEWS comment by Shaman J. An estimation of undetected COVID cases in France. Nature 2020, published 21 December. Full-text: https://www.nature.com/articles/d41586-020-03513-9
de Gier B, de Oliveira BL, van Gaalen RD, et al. Occupation- and age-associated risk of SARS-CoV-2 test positivity, the Netherlands, June to October 2020. Euro Surveill December 17, 2020;25(50):pii=2001884. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.50.2001884
This study from the Netherlands found an increased positivity to the COVID test among workers in the hospitality and public transport sectors, but also among driving instructors, hairdressers and estheticians.
22 December
Aschele C, Negru M, Pastorino A, et al. Incidence of SARS-CoV-2 Infection Among Patients Undergoing Active Antitumor Treatment in Italy. JAMA Oncol December 17, 2020; Full-text: https://doi.org/10.1001/jamaoncol.2020.6778
Large investigation on the incidence of SARS-CoV-2 in almost 60.000 patients with cancer. The 0,68% rate of infection was relatively low. Notably, the rate remained below 1% even in areas with the greatest COVID-19 spread, partly reflecting reorganization measures implemented in medical oncology units in Italy at the onset of this outbreak, supporting the continuation of most oncologic treatments in the adjuvant and metastatic setting. Based on these data, delaying active antitumor treatment to avoid SARS-CoV-2 transmission should not be routinely recommended.
17 December
Poustchi H, Darvisshiaqan M, Mohammadi Z, et al. SARS-CoV-2 antibody seroprevalence in the general population and high-risk occupational groups across 18 cities in Iran: a population-based cross-sectional study. Lancet Infect Dis December 15, 2020. Full-text: https://doi.org/10.1016/S1473-3099(20)30858-6
Seroprevalence is likely to be much higher than the reported prevalence of COVID-19 based on confirmed COVID-19 cases in Iran. The overall population weight-adjusted and test performance-adjusted prevalence of antibody seropositivity in the general population was 17.1% (95% CI 14.6–19.5). Despite high seroprevalence in a few cities, a large proportion of the population is still uninfected.
16 December
Mutambudzi M, Niedwiedz C, Macdonald EB, et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med. 2020 Dec 9:oemed-2020-106731. PubMed: https://pubmed.gov/33298533. Full-text: https://doi.org/10.1136/oemed-2020-106731
Essential workers such as healthcare workers (RR 7.43, 95% CI 5.52 to 10.00), social and education workers (RR 1.84, 95% CI 1.21 to 2.82) and other essential workers (RR 1.60, 95% CI 1.05 to 2.45) appear to have a higher risk of severe COVID-19. This is the result of a prospective cohort study of 120.075 persons, (employed or self-employed, alive and aged < 65 years in 2020), of whom 271 had severe COVID-19. We need to protect them!
Althoff KN, Laeyendecker O, Li R, et al. SARS-CoV-2 antibody status in decedents undergoing forensic postmortem examination in Maryland, May 24 to June 30, 2020. Open Forum Infect Dis 2020, published 15 December. Full-text: https://doi.org/10.1093/ofid/ofaa611
Seroprevalence of SARS-CoV-2 antibodies was 10% among the subset of decedents undergoing forensic post-mortem examination in June in Maryland. Decedents of motor vehicle crashes had similar seroprevalence compared to those with a natural death (including decedents with SARS-CoV-2 infection). Decedents of motor vehicle crashes may be a sentinel surveillance population.
15 December
Tracking the Coronavirus at U.S. Colleges and Universities. The New York Time 2020, published 11 December. Full-text: https://www.nytimes.com/interactive/2020/us/covid-college-cases-tracker.html
Harmon A. Superspreading Boston biotech conference in February is linked to 1.9 percent of all U.S. cases. The New York Times 2020, published 11 December. Full-text: https://www.nytimes.com/2020/12/11/world/superspreading-boston-biotech-conference-in-february-is-linked-to-1-9-percent-of-all-us-cases.html
A short summary of the study by Lemieux JE et al. we presented two days ago (Lemieux JE, Siddle KJ, Shaw BM, et al. Phylogenetic analysis of SARS-CoV-2 in Boston highlights the impact of superspreading events. Science 2020, published 10 December. Full-text: https://doi.org/10.1126/science.abe3261). As many as 300.000 coronavirus cases across the United States can be traced to a two-day conference in Boston convened by the drug company Biogen.
13 December
Buss LF, Prete Jr A, Abrahim CMM, et al. Three-quarters attack rate of SARS-CoV-2 in the Brazilian Amazon during a largely unmitigated epidemic. Science 2020, published 8 December. Full-text: https://doi.org/10.1126/science.abe9728
Brazil has experienced one of the world’s most rapidly-growing COVID-19 epidemics, with the Amazon being the worst hit region. Here, Ester Sabino, Nuno Faria, Lewis Buss and colleagues show that one month after the epidemic peak in Manaus, capital of Amazonas state, 44% of the population had detectable IgG antibodies. Correcting for cases without a detectable antibody response and antibody waning, the authors estimate a 66% attack rate in June, rising to 76% in October. The authors conclude that when poorly controlled, COVID-19 can infect a high fraction of the population causing high mortality.
Geoghegan JL, Ren X, Storey M, et al. Genomic epidemiology reveals transmission patterns and dynamics of SARS-CoV-2 in Aotearoa New Zealand. Nat Commun 11, 6351 (2020). Full-text: https://doi.org/10.1038/s41467-020-20235-8
New Zealand is one of a handful of countries that aimed to eliminate coronavirus disease 19 (COVID-19). Here, Jemma L. Geoghegan generated 649 SARS-CoV-2 genome sequences from infected patients with samples collected during the ‘first wave’, representing 56% of all confirmed cases in this time period. The authors found that only 19% of virus introductions into New Zealand resulted in ongoing transmission of more than one additional case. They conclude that ongoing genomic surveillance should be an integral part of the national response to monitor any re-emergence of the virus, particularly when border restrictions might eventually be eased.
12 December
Amendola A, Bianchi S, Gori M, Colzani D, Canuti M, Borghi E, et al. Evidence of SARS-CoV-2 RNA in an oropharyngeal swab specimen, Milan, Italy, early December 2019. Emerg Infect Dis 2020, published 8 December. Full-text: https://doi.org/10.3201/eid2702.204632
Elisabetta Tanzi, Antonella Amendola and colleagues from the University of Milan identified SARS-CoV-2 RNA in an oropharyngeal swab specimen collected from a child with suspected measles in early December 2019, more than two months before the first identified SARS-CoV-2 case in Italy. The authors cautiously conclude that “long-term, unrecognized spread of SARS-CoV-2 in northern Italy would help explain, at least in part, the devastating impact and rapid course of the first wave of COVID-19 in Lombardy.”
Pouwels KB, House T, Pritchard E, et al. Community prevalence of SARS-CoV-2 in England from April to November, 2020: results from the ONS Coronavirus Infection Survey. Lancet Public Health 2020, published 10 December. Full-text: https://doi.org/10.1016/S2468-2667(20)30282-6
Seroprevalence for SARS-CoV-2 continues to be low in England. After randomly collecting samples from individuals aged 2 years and older living in private households in England, the percentage of people testing positive for SARS-CoV-2 initially decreased between April 26 and June 28, 2020, from 0·40% to 0·06%, followed by low levels during July and August, 2020, before substantially increasing at the end of August, 2020, with percentages testing positive above 1% from the end of October, 2020. Age (young adults, particularly those aged 17–24 years) was an important initial driver in the second wave. For example, the estimated percentage of individuals testing positive was more than six times higher in those aged 17–24 years than in those aged 70 years or older at the end of September, 2020. More than half of infections were in asymptomatic individuals.
10 December
Ismail SA, Saliba V, Bernal JL, et al. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Inf Dis December 08, 2020. Full-text: https://doi.org/10.1016/S1473-3099(20)30882-3
In this prospective, cross-sectional analysis of educational settings in England that had re-opened after the first national lockdown, SARS-CoV-2 infections and outbreaks were uncommon. Among 55 outbreaks (at least two epidemiologically linked cases, with sequential cases diagnosed within 14 days in the same educational setting), probable direction of transmission was staff-to-staff in 26, staff-to-student in 8, student-to-staff in 16 outbreaks, and student-to-student in 5 outbreaks. The risk of an outbreak increased by 72% (95% CI 28–130) for every five cases per 100.000 population increase in community incidence, emphasizing the importance of controlling community transmission to protect educational settings. Interventions should focus on reducing transmission in and among staff.
See also the comment by Flasche S, Edmunds JW. The role of schools and school-aged children in SARS-CoV-2 transmission. The Lancet Infectious Diseases. December 8, 2020. Full-text: https://doi.org/10.1016/S1473-3099(20)30927-0
8 December
Haag C, Höglinger M, Moser A, et al. Social mixing and risk exposures for SARS-CoV-2 infections in elderly persons. Swiss Med Wkly. 2020 Dec 5;150:w20416. PubMed: https://pubmed.gov/33277915 . Full-text: https://doi.org/10.4414/smw.2020.20416
Although many elderly persons continued to follow the recommended preventive measures during the transitional phase between the two pandemic waves, social mixing with younger persons constitutes a way for transmission of infections across age groups. In this large survey from Switzerland, about one quarter of all elderly were still strictly adhering to social distancing and preventive measures. In contrast, a minority of 10% of the elderly had many social contacts and were lacking adherence to preventive measures. The remaining groups seemed to fall in between: while they did have multiple personal contacts, they did maintain the recommended distance. Thus, preventive measures remain important among all age groups.
Balabdaoui F, Mohr D. Age-stratified discrete compartment model of the COVID-19 epidemic with application to Switzerland. Sci Rep. 2020 Dec 4;10(1):21306. PubMed: https://pubmed.gov/33277545. Full-text: https://doi.org/10.1038/s41598-020-77420-4
A discrete modeling framework is proposed to capture the dynamics of highly age-sensitive epidemics and to evaluate the effect of social contact patterns on the load of hospitals and their intensive care units. According to the authors, there should be sufficient time for governments to take corrective measures in case they detect a significant increase in hospitalizations after relaxing the lockdown. Even though the second wave may not lead to a collapse of the healthcare system in Switzerland, it is still important to maintain the overall reproduction number always below one to avoid any silent multiplication of the total number of fatalities.
5 December
Epidemiology
Podewils LJ, Burket TL, Mettenbrink C, et al. Disproportionate Incidence of COVID-19 Infection, Hospitalizations, and Deaths Among Persons Identifying as Hispanic or Latino — Denver, Colorado March–October 2020. MMWR Morb Mortal Wkly Rep 2020;69:1812–1816. Full-text: http://dx.doi.org/10.15585/mmwr.mm6948a3
COVID-19 disproportionately affected Hispanic persons in Denver, US. Overall, the proportions of COVID-19 cases (55%), hospitalizations (62%), and deaths (51%) among Hispanic adults were approximately double the proportion of Hispanic adults in the Denver community (24,9%). Among adults with COVID-19, Hispanic persons reported larger household sizes and more known COVID-19 household exposure, working in essential industries, working while ill, and delays in testing after symptom onset.
Horton R. Offline: COVID-19—what have we learned so far? Lancet 2020, published 5 December. Full-text: https://doi.org/10.1016/S0140-6736(20)32584-8
Richard Horton, the Lancet Editor-in-Chief, briefly discusses what we have discovered in 2020 and how these discoveries might inform our future.
2 Dezember
Guerriero M, Bisoffi Z, Poli A, Micheletto C, Conti A, Pomari C. Prevalence of SARS-CoV-2, Verona, Italy, April–May 2020. Emerg Infect Dis. 2021 Jan. Full-text: https://doi.org/10.3201/eid2701.202740
In Veneto, Italy, Verona was the province with the most cases and deaths caused by SARS-CoV-2. Massimo Guerriero and colleagues estimated the prevalence of active or past infection among randomly selected participants > 10 years of age from Verona. Of 1515 participants, 2,6% tested positive by a serologic assay and 0,7% by PCR. The total prevalence was 3,0%, suggesting 7051 cumulative cases (4,6 times higher than the official count).
1 Dezember
Yoon Y, Choi G-J, Kim JY, Kim K-R, Park H, Chun JK, et al. Childcare exposure to severe acute respiratory syndrome coronavirus 2 for 4-year-old presymptomatic child, South Korea. Emerg Infect Dis 2020 November 30, 2020. Full-text: https://doi.org/10.3201/eid2702.203189
An epidemiologic investigation of potential exposure of a presymptomatic child who attended a childcare center in South Korea: a 4-year-old child, probably infected by his grandmother, attended the center during the presymptomatic period (February 19–21, 2020). Fever developed on February 22, and he was given a diagnosis of SARS-CoV-2 infection on February 27. At the center, 190 persons were identified as contacts; 44 (23.2%) were defined as close contacts (37 children and 7 adults). All 190 persons were negative for SARS-CoV-2 on days 8–9 after the last exposure. This investigation adds indirect evidence of potentially low infectivity in a childcare setting with exposure to a presymptomatic child.
30 November
Vos ERA, den Hartog G, Schepp RM, et al. Nationwide seroprevalence of SARS-CoV-2 and identification of risk factors in the general population of the Netherlands during the first epidemic wave. J Epidemiol Community Health. 2020 Nov 28:jech-2020-215678. PubMed: https://pubmed.gov/33249407. Full-text: https://doi.org/10.1136/jech-2020-215678
During the first wave of the epidemic in April 2020, overall seroprevalence in the Netherlands was 2,8% (95% CI 2.1 to 3.7), with no differences between sexes or ethnic background, and regionally ranging between 1,3 and 4,0%. This is in striking contrast with the 30-fold lower number of reported cases.
29 November
Trieu MC, Bansal A, Madsen A, et al. SARS-CoV-2-specific neutralizing antibody responses in Norwegian healthcare workers after the first wave of COVID-19 pandemic: a prospective cohort study. J Infect Dis. 2020 Nov 28:jiaa737. PubMed: https://pubmed.gov/33247924 . Full-text: https://doi.org/10.1093/infdis/jiaa737
A low number of SARS-CoV-2-seropositive HCWs in a low prevalence setting. In this study from Norway, 607 HCW were evaluated pre- and post-the first COVID-19 pandemic wave, using a 2-step ELISA. Exposure history, COVID-19-like symptoms and serum samples were collected. Only 32 HCW (5.3%) had spike-specific antibodies (11 seroconverted with ≥ 4-fold increase, 21 were seropositive at baseline). The infection rate was only 1,7-fold higher in HCW with COVID-19 patient-exposure (2,4%) than in HCW with no exposure (1,4%).
Santos-Hövener C, Neuhauser HK, Schaffrath Rosario A, et al, CoMoLo Study Group. Serology- and PCR-based cumulative incidence of SARS-CoV-2 infection in adults in a successfully contained early hotspot (CoMoLo study), Germany, May to June 2020. Euro Surveill. 2020;25(47):pii=2001752. https://doi.org/10.2807/1560-7917.ES.2020.25.47.2001752
After a large church concert on March 1 and the first detected infection on March 9, the southern German community of Kupferzell in the federal state Baden-Württemberg faced a steep increase of SARS-CoV-2 infections. The cumulative incidence of 1.760 per 100.000 by the end of April was one of the highest in Germany. The authors set out to analyze the SARS-CoV-2 seroprevalence in a random sample of this community from 20 May to 9 June. Results: 12%. This study confirmed that even in areas with high COVID-19 prevalence, only a small proportion of the population is infected.
28 November
Muiry R, Parsons V, Madan I. Risks posed by COVID-19 to healthcare workers. Occup Med 2020, published 28 November. Full-text: https://doi.org/10.1093/occmed/kqaa191
What is the exact nature of the risks posed by SARS-CoV-2 to healthcare workers? Rupert Muiry, Vaughan Parsons and Ira Madan summarize the current literature, including consideration of broader biopsychosocial morbidities.
Bajema K, Wiegand RE, Cuffe K, et al. Estimated SARS-CoV-2 Seroprevalence in the US as of September 2020. JAMA Intern Med 2020, published 24 November. Full-text: https://doi.org/10.1001/jamainternmed.2020.7976
In this cross-sectional study of 177.919 clinical specimens, Chris Edens, Kristina Bajema and colleagues found that as of September 2020, fewer than 10% of people had detectable SARS-CoV-2 antibodies. Seroprevalence estimates varied between sexes, across age groups, and between metropolitan/non-metropolitan area.
27 November
Mavragani A, Gkillas K. COVID-19 predictability in the United States using Google Trends time series. Sci Rep 10, 20693 (2020). Full-text: https://doi.org/10.1038/s41598-020-77275-9
How will you monitor and forecast regional outbreaks as they happen or even before they happen? By using Google Trends. Amaryllis Mavragani and Konstantinos Gkillas from the University of Stirling in Scotland present a model that exhibits strong COVID-19 predictability. The authors conclude that Google Trends offers a solid foundation for quantitative analysis with respect to the monitoring and predictability of COVID-19 and suggest that these approaches may flatten epidemic curves, help in allocating health resources, and increase the effectiveness and preparedness of health care systems.
26 November
Kuehn BM. Hand Hygiene Gaps Identified. JAMA. 2020 Nov 24;324(20):2021. PubMed: https://pubmed.gov/33231672. Full-text: https://doi.org/10.1001/jama.2020.22227
Men, young adults, and White people are more likely than other groups to be too stupid to wash their hands properly. Bridget Kuehn reminds us of a pair of surveys published in MMWR (Haston 2020; Czeisler 2020, presented 21 June) that found serious gaps in hand hygiene practices by race, age, and sex. Hand washing or using an alcohol-based hand sanitizer after touching shopping carts, gas pumps, automated teller machines, etc. – tell your boys, tell your men, tell your white neighbors.
25 November
Bajema KL, Wiegand RE, Cuffe K, et al. Estimated SARS-CoV-2 Seroprevalence in the US as of September 2020. JAMA Intern Med November 24, 2020. Full-text: https://doi.org/10.1001/jamainternmed.2020.7976
In this repeated, cross-sectional study of 177.919 residual clinical specimens, the estimated percentage of persons in a US jurisdiction with detectable SARS-CoV-2 antibodies ranged from fewer than 1% to 23%. Over 4 sampling periods in 42 of 49 jurisdictions with calculated estimates, fewer than 10% of people had detectable SARS-CoV-2 antibodies.
Kennedy BS, Richeson RP, Houde AJ. Risk Factors for SARS-CoV-2 in a Statewide Correctional System. N Eng J Med November 24, 2020. Full-text: https://doi.org/10.1056/NEJMc2029354
Mass testing by RT-PCR among 10.304 incarcerated persons in the Connecticut (US) statewide correctional system revealed that by far the strongest risk factor for SARS-CoV-2 infection was dormitory housing (odds ratio, 35.3). Social distancing may be more challenging in such settings than in cells that house one or two inmates.
Liu M, Thomadsen R, Yao S. Forecasting the spread of COVID-19 under different reopening strategies. Sci Rep 10, 20367 (2020). Full-text: https://doi.org/10.1038/s41598-020-77292-8
Using a modified susceptible-infected-recovered (SIR) model in the United States, the authors found that the incidence of COVID-19 spread is concave in the number of infectious individuals, as would be expected if people have inter-related social networks. This concave shape has a significant impact on forecasted COVID-19 cases. The number of COVID-19 cases would only have an exponential growth for a brief period at the beginning of the contagion event or right after a re-opening, but would quickly settle into a prolonged period of time with stable, slightly declining levels of disease spread. In contrast, if social distancing is eliminated, there will be a massive increase in the cases.
24 November
Jeong JM, Radeos MS, Shee B, et al. COVID-19 Seroconversion in Emergency Professionals at an Urban Academic Emergency Department in New York City. Ann Emerg Med. 2020 Dec;76(6):815-816. PubMed: https://pubmed.gov/33222793. Full-text: https://doi.org/10.1016/j.annemergmed.2020.06.038
Emergency professionals as a high-risk group. Between February 1, 2020, and April 30, 2020, an overwhelming number greater than 1,000 patients with a diagnosis of COVID-19 presented at an emergency department (ED) in Brooklyn, NY. Results: The overall rate of seroconversion among emergency professionals was incredibly high (46%). Rates for attending physicians, emergency medicine residents, and physician assistants were 64%, 36%, and 29%, respectively.
23 November
Taylor CA, Boulos C, Almond D. Livestock plants and COVID-19 transmission. PNAS November 19, 2020. Full-text: https://doi.org/10.1073/pnas.2010115117
Livestock processing poses a particular public health risk extending far beyond meatpacking companies and their employees. The authors estimate livestock plants to be associated with 236.000 to 310.000 COVID-19 cases (6 to 8% of total US cases) and 4300 to 5.200 deaths (3 to 4% of total US cases) as of July 21. They also illustrate potential contributions of plant size, industrial concentration, plant shutdowns, and policy actions to this phenomenon. High numbers were found among large processing facilities and large meatpacking companies. According to the authors, their results “motivate investigation into supply chains, operating procedures, and labor relations within the meatpacking industry”. They also discuss some implications. Interestingly, one was seemingly beyond the intellectual grasp of the authors: that consumers could abstain from buying meat produced by these large meatpacking companies.
22 November
Thompson CN, Baumgartner J, Pichardo C, et al. COVID-19 Outbreak — New York City, February 29–June 1, 2020. MMWR 2020;69:1725–1729. Full-text: http://dx.doi.org/10.15585/mmwr.mm6946a2
During March–May 2020, approximately 203.000 laboratory-confirmed COVID-19 cases were reported to the NYC Department of Health and Mental Hygiene (DOHMH). The crude fatality rate (CFR) among confirmed cases was 9.2% overall and 32.1% among hospitalized patients. Incidence, hospitalization rates, and mortality were highest among Black/African American and Hispanic/Latino persons, as well as those who were living in neighborhoods with high poverty, aged ≥ 75 years, and with underlying medical conditions. Of note, the overall CFR of 9,2% is an overestimate because of under-ascertainment of cases, given the restrictive testing guidance and limited availability of tests during the first 2 months of the epidemic.
21 November
Firestone MJ, Wienkes H, Garfin J, et al. COVID-19 Outbreak Associated with a 10-Day Motorcycle Rally in a Neighboring State — Minnesota, August–September 2020. MMWR Morb Mortal Wkly Rep. ePub: 20 November 2020. DOI: http://dx.doi.org/10.15585/mmwr.mm6947e1
August 2020? Too soon for news about SARS-CoV-2 to have spread through western South Dakota, USA. Unaware of the pandemic, approximately 460.000 persons attended a motorcycle rally with numerous indoor and outdoor events over a 10-day period. The results: 51 confirmed primary event-associated cases, 21 secondary cases, and five tertiary cases. An additional nine likely rally-associated secondary or tertiary cases occurred. Four patients were hospitalized, and one died.
Cao S, Gan Y, Wang C, et al. Post-lockdown SARS-CoV-2 nucleic acid screening in nearly ten million residents of Wuhan, China. Nat Commun 11, 5917 (2020). Full-text: https://doi.org/10.1038/s41467-020-19802-w
Which government wouldn’t like to have correct estimates of the prevalence of SARS-CoV-2 infection following the release of lockdown restrictions? Here is what happened in Wuhan between May 14 and June 1, 2020, where authorities ordered a city-wide SARS-CoV-2 screening program. All city residents aged six years or older were eligible and 9.899.828 (92,9%) participated. No new symptomatic cases and 300 asymptomatic cases (detection rate 0,303/10.000) were identified. There were no positive tests amongst 1174 close contacts of asymptomatic cases.
Al-Mandhari AS, Brennan RJ Abubakar A, Hajjeh R. Tackling COVID-19 in the Eastern Mediterranean Region. Lancet 2020, published 19 November. Full-text: https://doi.org/10.1016/S0140-6736(20)32349-7
Most countries in the Eastern Mediterranean region saw fairly slow transmission of SARS-CoV-2 during the early months of the pandemic but in May, as social measures, such as restrictions and partial or full lockdowns, were relaxed during the holy month of Ramadan, disease transmission accelerated.
20 November
Van Dorp L, Tan CCS, Datt Lam S, et al. Recurrent mutations in SARS-CoV-2 genomes isolated from mink point to rapid host-adaptation. bioRxiv 2020, posted 16 November. Full-text: https://doi.org/10.1101/2020.11.16.384743
If you introduce SARS-CoV-2 in mink farms, it spreads and mutates rapidly. This is the result of a study which looked into 239 viral genomes isolated from farmed animals in the Netherlands and Denmark. The authors identified 23 recurrent mutations including three mutations in the Receptor Binding Domain of the SARS-CoV-2 spike protein that independently emerged at least four times but are only rarely observed in human lineages. Reassuringly, the authors state that the low prevalence of mink-adapted mutations in strains circulating in humans to date (November 2020) suggests that they are not expected to increase transmission of SARS-CoV-2 in humans.
19 November
Xing Y, Wong GWK, Ni W, Hu X, Xing Q. Rapid Response to an Outbreak in Qingdao, China. N Engl J Med 2020, published 18 November. Full-text: https://doi.org/10.1056/NEJMc2032361
Three COVID-19 cases in Qingdao in October: a taxi driver who was admitted to Qingdao Central Hospital for a transient ischemic attack on October 10; his wife who had been working part-time as a nursing assistant at Qingdao Chest Hospital; and a man with pulmonary tuberculosis who was treated at the same hospital. These were the first cases after a 2-month period without local SARS-CoV-2 transmission in China. What would you have done during the next 7 days? The Chinese authorities tested 10.9 million people and identified another 9 cases related to the initial cluster. The outbreak was controlled without a lockdown.
18 November
Denny TN, Andrews L, Bonsignori M, et al. Implementation of a Pooled Surveillance Testing Program for Asymptomatic SARS-CoV-2 Infections on a College Campus — Duke University, Durham, North Carolina, August 2–October 11, 2020. MMWR Morb Mortal Wkly Rep. ePub: 17 November 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6946e1
Test them all? In fall 2020, Duke University’s COVID-19 prevention strategy included risk reduction behaviors, but also frequent testing using pooled SARS-CoV-2 PCR testing, and contact tracing. Of 10,265 students who received testing 68,913 times, 84 had positive results. Of these, 51% were asymptomatic, and some had high viral loads. This plan allowed campus to remain open for 10 weeks of classes without substantial outbreaks among residential or off-campus populations. Importantly, no evidence from contact tracing linked transmission with in-person classes. Pooled testing permitted a nearly 80% savings in use of reagents and laboratory resources compared with testing each individual specimen.
17 November
Mahale P, Rothfuss C, Bly S, et al. Multiple COVID-19 Outbreaks Linked to a Wedding Reception in Rural Maine — August 7–September 14, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1686–1690. Full-text: http://dx.doi.org/10.15585/mmwr.mm6945a5
Do you have a niece who, despite all the warnings, is unwaveringly sticking to her plans to get married in January? Who says that only 50 guests (ok, 55) will come and that temperature checks for all guests will be conducted at the facility entrance? That there will be enough space, with 10 tables, with 4–6 guests seated around each table? That signs posted at the entrance will instruct visitors to wear masks? Then give her this paper to read. A wedding reception in a small rural town in Maine was the likely source of COVID-19 outbreaks in the local community, a long-term care facility, and a correctional facility. Outcome: 177 cases, seven hospitalizations, and seven deaths. Read here why people should avoid large gatherings, practice physical distancing, wear masks, stay home when ill, and self-quarantine after exposure to a person with confirmed SARS-CoV-2 infection.
(If your niece doesn’t want to read a scientific paper, provide her with “15 Benefits of A Summer Wedding”: https://www.nichemarket.co.za/blog/extravaganza/benefits-summer-wedding. Benefit No. 16 is found probably below, in the vaccine section.)
Ali H, Kondapally K, Pordell P, et al. COVID-19 Outbreak in an Amish Community — Ohio, May 2020. MMWR Morb Mortal Wkly Rep 2020;69:1671–1674. Full-text: http://dx.doi.org/10.15585/mmwr.mm6945a2
How social gatherings likely contributed to rapid transmission of SARS-CoV-2 in an Amish community. In May, after a cluster of seven COVID-19 cases was identified, 23/30 (77%) additional residents tested by RT-PCR received positive test results. Rapid and sustained transmission of SARS-CoV-2 was associated with multiple social gatherings. Although Amish communities might be experiencing challenges with preventing and mitigating SARS-CoV-2 transmission, the authors conclude that leveraging Amish cultural beliefs of communal responsibility could help limit the spread of SARS-CoV-2.
Wang EA, Western B, Berwick DM. COVID-19, Decarceration, and the Role of Clinicians, Health Systems, and Payers. A Report From the National Academy of Sciences, Engineering, and Medicine. JAMA November 16, 2020. Full-text: https://doi.org/10.1001/jama.2020.22109
By August 2020, 90 of the largest 100 cluster outbreaks in the United States had occurred in prisons and jails. Reducing the incarcerated population (“decarceration”) is an important and urgent strategy for mitigating viral transmission in prisons and jails. In their courageous viewpoint, Emily Wang and colleagues argue that decarceration in the service of both public health and safer communities will require sustained engagement from clinicians, health systems, and Medicaid authorities.
15 November
Brotons P, Launes C, Buetas E, et al. Susceptibility to Sars-COV-2 Infection Among Children And Adults: A Seroprevalence Study of Family Households in the Barcelona Metropolitan Region, Spain. Clinical Infectious Diseases, November 12, 2020. Full-text: https://doi.org/10.1093/cid/ciaa1721
Children have similar probability as adults to become infected by SARS-CoV-2 in quarantined family households. Pedro Brotons and colleagues from Barcelona performed a large cross-sectional seroprevalence study, enrolling 381 family households including 381 first-reported PCR-positive adult cases and 1084 contacts (672 children, 412 adults). SARS-CoV-2 infection seroprevalence rates were 18% (118/672) in children and 19% (77/335) in adult contacts. Nearly all positive pediatric contacts were asymptomatic or had mild symptoms.
Ebrahim SH, Ahmed Y, Algahtani SA, et al. The Hajj pilgrimage during the COVID-19 pandemic in 2020: event hosting without the mass gathering. Journal of Travel Medicine November 13, 2020. Full-text: https://academic.oup.com/jtm/advance-article/doi/10.1093/jtm/taaa194/5979518
Examples of religious congregations that resulted in seeding or surging of domestic and international COVID-19 outbreaks include events in Daegu, South Korea; Qom, Iran; Albany, Georgia; Arkansas + Maine, USA; and Mulhouse, France. Read how the science-driven steering of the 2020 Hajj with vastly reduced pilgrim numbers allowing for full compliance of the mitigation strategies avoided the cancellation of the event.
14 November
Malani A, Shah D, Kang G, et al. Seroprevalence of SARS-CoV-2 in slums versus non-slums in Mumbai, India. Lancet Global Health 2020, published 13 November. Full-text: https://doi.org/10.1016/S2214-109X(20)30467-8
This is the final article of a pre-print study we presented on August 4: Kolthur-Seetharam U, Shah D, Shastri J, Juneja S, Kang G, Malani A, Mohanan M, Lobo GN, Velhal G, Gomare M. SARS-CoV2 Serological Survey in Mumbai by NITI-BMC-TIFR. Tata Institute of Fundamental Research (TIFR) 2020, published 29 June. Full-text: https://www.tifr.res.in/TSN/article/Mumbai-Serosurvey%20Technical%20report-NITI.pdf
“We usually prefer peer-reviewed studies and seldom present pre-published papers. We are even less readily inclined to present a PDF with just the technical details of an unpublished study. Today we make an exception. In a cross-sectional survey in Mumbai, India, Ullas Kolthur-Seetharam and colleagues estimated the prevalence of SARS-CoV-2 infection in three Mumbai areas (called ‘wards’) in July 2020. The authors found, on average, a prevalence of around 57% in the slum areas of Chembur, Matunga and Dahisar, and 16% in neighboring non-slums. If these data are confirmed, some Mumbai areas would soon reach herd immunity and could return to a pre-COVID way of life.”
See also a short comment in The Economist. Anonymous. A minority of people with covid-19 account for the bulk of transmission. The Economist 2020, published 7 November. Full-text: https://www.economist.com/graphic-detail/2020/11/07/a-minority-of-people-with-covid-19-account-for-the-bulk-of-transmission
13 November
Uyoga S, Adetifa IMO, Karanja HK, et al. Seroprevalence of anti–SARS-CoV-2 IgG antibodies in Kenyan blood donors. Science 2020, published 11 November. Full-text: https://doi.org/10.1126/science.abe1916
In April-June 2020, the crude prevalence of anti–SARS-CoV-2 IgG among blood donors in Kenya was 5,6% (174/3098). It was highest in urban counties, Mombasa (8,0%), Nairobi (7,3%) and Kisumu (5,5%). Of note, Kenya reported only 341 deaths by the end of that period. The authors conclude that the sharp contrast between the reported COVID-19 cases and deaths suggests that the disease might be attenuated in Africa.
Waterfield T, Watson C, Moore R, et al. Seroprevalence of SARS-CoV-2 antibodies in children: a prospective multicentre cohort study. Arch Dis Child. 2020 Nov 10:archdischild-2020-320558. PubMed: https://pubmed.gov/33172887. Full-text: https://doi.org/10.1136/archdischild-2020-320558
Fatigue, gastrointestinal symptoms and changes in sense of smell or taste were the symptoms most strongly associated with SARS-CoV-1 antibody positivity in children. Thomas Waterfield et al. report 68/992 (6,9%) children aged 2-15 years with positive SARS-CoV-2 antibody tests. Of these, 34/68 (50%) reported no symptoms prior to testing. Four independent variables were identified as significantly associated with SARS-CoV-2 seropositivity: known infected household contact OR=10,9; fatigue OR=16,8; gastrointestinal symptoms OR=6,6; and changes in sense of smell or taste OR=10,0.
Slot E, Hogema BM, Reusken CBEM, et al. Low SARS-CoV-2 seroprevalence in blood donors in the early COVID-19 epidemic in the Netherlands. Nat Commun 11, 5744 (2020). Full-text: https://doi.org/10.1038/s41467-020-19481-7
One month into the outbreak and more than 2 weeks after social distancing and lockdown interventions were implemented, the proportion of SARS-CoV-2 antibody-positive individuals in the Dutch population tested was 2,7%. Hans Zaaijer, Ed Slot and colleagues also demonstrate that the hardest-hit areas had a seroprevalence of up to 9,5%; the seroprevalence was sex-independent throughout age groups (18–72 years); and antibodies were significantly more often present in young people aged 18–30 years.
11 November
Kurian SJ, Bhatti AUR, Alvi MA, et al. Correlations Between COVID-19 Cases and Google Trends Data in the United States: A State-by-State Analysis. Mayo Clin Proc. 2020 Nov;95(11):2370-2381. PubMed: https://pubmed.gov/33164756. Full-text: https://doi.org/10.1016/j.mayocp.2020.08.022
Google might see a nascent epidemic two weeks before the first reported cases. This is the result of a study by Mohamad Bydon, Shyam J. Kurian and colleagues from Mayo Clinic, Rochester after developing a digital surveillance model using Google Trends. The authors searched the following keywords: COVID symptoms, coronavirus symptoms, sore throat+shortness of breath+fatigue+cough, coronavirus testing center, loss of smell, Lysol (sanitizer), antibody, face mask, coronavirus vaccine, and COVID stimulus check. Find out which one did best. The authors suggest that this information could enable better preparation and planning for health care systems.
10 November
Brown KA, Jones A, Daneman N, et al. Association Between Nursing Home Crowding and COVID-19 Infection and Mortality in Ontario, Canada. JAMA Intern Med. November 9, 2020. Full-text: https://doi.org/10.1001/jamainternmed.2020.6466
In this cohort study that included 78,607 residents of 618 nursing homes in Ontario, Canada, 5218 (6.6%) developed COVID-19 infection and 1452 (1.8%) died of COVID-19 infection as of May 20, 2020. The case fatality rate was 27.8% (1452/5218). Of note, COVID-19 mortality in homes with low crowding (number of occupants per room and bathroom across an entire home) was less than half (1.3%) than that of homes with high crowding (2.7%).
9 November
Siegenfeld AF, Bar-Yam Y. The impact of travel and timing in eliminating COVID-19. Commun Phys 3, 204 (2020). Full-text: https://doi.org/10.1038/s42005-020-00470-7
Mathematical models show that these are not good times for travel. When a reduction in travel is coupled with other control measures, the travel reduction will not only delay the spread of the outbreak but in some cases will also be the determining factor in whether or not the outbreak is eliminated.
Kanu FA, Smith EE, Offutt-Powell T, et al. Declines in SARS-CoV-2 Transmission, Hospitalizations, and Mortality After Implementation of Mitigation Measures— Delaware, March–June 2020. MMWR Morb Mortal Wkly Rep. ePub: 6 November 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6945
No single mitigation strategy is likely to be effective alone: state-mandated stay-at-home orders and public mask mandates coupled with case investigations and contact tracing contributed to an 82% reduction in COVID-19 incidence, 88% reduction in hospitalizations, and 100% reduction in mortality in Delaware during late April–June.
5 November
Pozzer A, Dominici F, Haines A, et al. Regional and global contributions of air pollution to risk of death from COVID-19. Cardiovasc Res 2020, published 26 October. Full-text: https://doi.org/10.1093/cvr/cvaa288
Air pollution might be an important cofactor increasing the risk of mortality from COVID-19. Jos Lelieveld, Andrea Pozzer and colleagues characterized global exposure to fine particulates based on satellite data and estimate that particulate air pollution contributed around 15% to COVID-19 mortality worldwide (East Asia, 27%; Europe, 19%; North America, 17%).
4 November
O’Driscoll M, Dos Santos GR, Wang L, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature (2020). Full-text: https://doi.org/10.1038/s41586-020-2918-0
The age distribution of deaths in younger age groups (<65 years) is consistent across different settings. This is the result of a study by Henrik Salje, Megan O’Driscoll and colleagues who used age-specific COVID-19 death data from 45 countries and the results of 22 seroprevalence studies to investigate the fatality patterns across multiple countries. The authors also demonstrate how outbreaks in nursing homes can drive overall population IFRs infection-to-fatality ratio), through both increased attack rates and increased vulnerability. They estimate that around 5% of the populations had been infected by the 1st of September 2020, with much higher transmission likely to have occurred in a number of Latin American countries.
Vijayan T, Shin M, Adamson PC, et al. Beyond the 405 and the 5: Geographic variations and factors associated with SARS-CoV-2 positivity rates in Los Angeles County. Clin Infect Dis 2020, published 3 November. Full-text: https://doi.org/10.1093/cid/ciaa1692
SARS-CoV-2 infection was more frequent in communities with high proportions of Latino/a residents, those living below the federal poverty line and with high household densities. This is the conclusion of a study by Tara Vijayan et al. in Los Angeles County (LAC) after analyzing more than 800,000 SARS-CoV-2 tests. The overall positivity rate was 10.2%.
30 October
Bassi F, Arbia G, Falorsi PD. Observed and estimated prevalence of Covid-19 in Italy: How to estimate the total cases from medical swabs data. Sci Total Environ. 2020 Oct 8:142799. PubMed: https://pubmed.gov/33066965. Full-text: https://doi.org/10.1016/j.scitotenv.2020.142799
A national survey in Italy from May to July 2020 found a nationwide seropositivity rate of 2.5% (Sabbadini 2020). Insiders never believed these figures and favored a seropositivity rate of 5-10% like in Spain or in France. Now we have a new estimate of COVID-19 prevalence in Italy by Francesca Bassi and colleagues: 9%, corresponding to almost 6 million Italians.
Pasco RF, Fox SJ, Jonston SC, et al. Estimated Association of Construction Work With Risks of COVID-19 Infection and Hospitalization in Texas. JAMA Netw Open 2020, published 29 October. Full-text: https://doi.org/10.1001/jamanetworkopen.2020.26373
In central Texas, US, construction work is associated with increased community transmission of SARS-CoV-2. This study found that resuming construction work during shelter-in-place orders was associated with increased transmission in the surrounding community. Construction workers had a nearly 5-fold increased risk of hospitalization compared with other occupational categories.
27 October
Bedford J, Enria D, Giesecke J, et al. Living with the COVID-19 pandemic: act now with the tools we have. Lancet 2020, published 24 October. Full-text: https://doi.org/10.1016/S0140-6736(20)32117-6
Let’s face reality: at the beginning of the second wave of the pandemic, we have some steroids which have been shown to reduce mortality in patients with severe COVID-19 (see Corticosteroids); and then we have a drug (remdesivir, Veklury®), which had a marginal benefit in a company-sponsored trial. That’s the COVID-19 treatment armamentarium as of October 2020 (see COVID Reference: Treatment). David Heymann, Juliet Bedford and colleagues summarize how to get through the 2020/2021 winter with what we have.
Kambhampati AK, O’Halloran AC, Whitaker M, et al. COVID-19–Associated Hospitalizations Among Health Care Personnel — COVID-NET, 13 States, March 1–May 31, 2020. MMWR Morb Mortal Wkly Rep. ePub: 26 October 2020. DOI: http://dx.doi.org/10.15585/mmwr.mm6943e3
Healthcare personnel (HCP) can have severe COVID-19–associated illness. In this analysis of 13 sites representing 98 counties in 13 states (California, Colorado, Connecticut, Georgia, Maryland, Michigan, Minnesota, New Mexico, New York, Ohio, Oregon, Tennessee, and Utah), Anita Kambhampati et al. show that 6% of 6760 adults hospitalized with COVID-19 from March 1–May 31, were HCP. Among HCP hospitalized with COVID-19, 36% were in nursing-related occupations, and 73% had obesity. Approximately 28% of these patients were admitted to an intensive care unit, 16% required invasive mechanical ventilation, and 4% died.
25 October
Mallapaty S. Why COVID outbreaks look set to worsen this winter. Nature News, October 23, 2020. Full-text: https://doi.org/10.1038/d41586-020-02972-4
It’s too soon to say whether COVID is seasonal like the flu — but where clusters aren’t under control, infections will continue to swell. Smriti Mallapaty explains how a small seasonal effect will probably contribute to bigger outbreaks in winter. Difficult months ahead.
Rafiei Y, Mello MM. The Missing Piece — SARS-CoV-2 Testing and School Reopening. October 21, 2020. Full-text: https://doi.org/10.1056/NEJMp2028209
Many health authorities (including the CDC) still recommend against screen testing in schools, citing constraints on testing capacity and the unavailability of real-world studies of its effectiveness. They focus on screening for COVID-19 symptoms. In this important viewpoint, Yasmin Rafiei and Michelle M. Mello explain why this will not work. They believe that increasing routine screening using rapid tests in schools should rank among the most urgent national priorities. Nevertheless, the testing-related challenges are immense (financial, logistics etc.). See above.
24 October
Guzzetta G, Riccardo F, Marziano V, Poletti P, Trentini F, Bella A, et al. Impact of a nationwide lockdown on SARS-CoV-2 transmissibility, Italy. Emerg Infect Dis. 2021 Jan. Full-text: https://doi.org/10.3201/eid2701.202114
While preparing for the next lockdown, let’s keep in mind that it worked during the first wave. The national lockdown put in place on March 11 in Italy brought the net (Rt) reproduction numbers below 1 in most regions and provinces within 2 weeks. Although Rt had been declining steeply even before the national lockdown in regions with intense interventions, Giorgio Guzzetta and colleagues estimate that the epidemic was brought under control only after the implementation of the lockdown. In addition, lockdown was fundamental to prevent an explosion in the number of cases in other regions in which transmission had started weeks later compared to the outbreak epicenters in Lombardy, Veneto and Emilia Romagna.
23 October
Aschwanden C. The false promise of herd immunity for COVID-19. Nature News Feature October 21. Full-text: https://doi.org/10.1038/d41586-020-02948-4
Herd immunity has recently been discussed as a desirable result of wide-scale vaccination programs. (High levels of vaccination-induced immunity in the population benefits those who can’t receive or sufficiently respond to a vaccine, such as people with compromised immune systems.) However, discussing herd immunity as a tool in the absence of vaccines has never been heard of before the SARS-CoV-2 pandemic. If you are tired and frustrated with distancing, lockdown and curfews and tempted by the notion of herd immunity (better: ‘herd protection’), read this brilliant article by Nature’s leading science writer Christie Aschwanden. Find out why proposals to largely let the virus run its course — embraced by Donald Trump’s administration and others — could bring untold death and suffering. Seasonal coronaviruses that cause common colds provoke a waning immunity that seems to last approximately a year. Until proof of the contrary, we should assume immunity to SARS-CoV-2 to be comparable. Without vaccines there will be no herd immunity for the foreseeable future.
Adlhoch C, Pebody R. What to expect for the influenza season 2020/21 with the ongoing COVID-19 pandemic in the World Health Organization European Region. Euro Surveill. 2020;25(42):pii=2001816. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.42.2001816
Less flu cases in this season? The positivity rate of 0.2% in the 2020 inter-seasonal period was lower than the average (1.1%) observed over the previous five inter-seasonal periods. However, although COVID-19 prevention and control measures will also support influenza prevention, influenza remains a threat to human health and a potential burden on the healthcare system.
22 October
Smith GD, Blastland M, Munafò M. Covid-19’s known unknowns. BMJ 2020;371:m3979. Full-text: https://www.bmj.com/content/371/bmj.m3979
Do we know exactly what’s going on with SARS-CoV-2 and exactly what to do about it? Over the past months, we have seen strongly contrasting but apparently equally authoritative statements about almost any topic. Stop the nonsense, write Georges Davey-Smith and his colleagues. Acknowledging uncertainty a little more might improve not only the atmosphere of the debate and the science, but also public trust. In any case, the more certain someone is about COVID-19, the less you should trust them.
19 October
Moozhipurath RK, Kraft L, Skiera B. Evidence of protective role of Ultraviolet-B (UVB) radiation in reducing COVID-19 deaths. Sci Rep 10, 17705 (2020). Full-text: https://doi.org/10.1038/s41598-020-74825-z
Serious? The authors applied a fixed-effect log-linear regression model to a panel dataset of 152 countries over 108 days (n = 6524). They used the cumulative number of COVID-19 deaths and case-fatality rate (CFR) as the main dependent variables and isolated the ultraviolet index (UVI) effect from potential confounding factors. After controlling for time-constant and time-varying factors, the authors found a significant negative association between UVI and COVID-19 deaths, indicating evidence of the protective role of ultraviolet B (UVB) in mitigating COVID-19 deaths. If confirmed via clinical studies, then the possibility of mitigating COVID-19 deaths via sensible sunlight exposure or vitamin D intervention would be highly attractive.
15 October
Alwan NA, Burgess RA, Ashworth S, et al. Scientific consensus on the COVID-19 pandemic: we need to act now. Lancet 2020, published 15 October. Full-text: https://doi.org/10.1016/S0140-6736(20)32153-X
Herd immunity against SARS-CoV-2? Allowing large uncontrolled outbreaks in the low-risk population while protecting the vulnerable? Developing population immunity in the low-risk population, which will eventually protect the vulnerable? The authors don’t beat about the bush: “Dangerous fallacy unsupported by scientific evidence.” Their conclusion: “Japan, Vietnam, and New Zealand, to name a few countries, have shown that robust public health responses can control transmission, allowing life to return to near-normal, and there are many such success stories. The evidence is very clear: controlling community spread of COVID-19 is the best way to protect our societies and economies until safe and effective vaccines and therapeutics arrive within the coming months. We cannot afford distractions that undermine an effective response; it is essential that we act urgently based on the evidence.”
Poirier C, Luo W, Majumder MS, et al. The role of environmental factors on transmission rates of the COVID-19 outbreak: an initial assessment in two spatial scales. Sci Rep 10, 17002 (2020). Full-text: https://doi.org/10.1038/s41598-020-74089-7
Bad news for CCOs (‘Coronavirus Climate Optimists’): changes in weather (i.e., increase of temperature and humidity as spring and summer months arrive in the Northern Hemisphere) may not necessarily lead to declines in case counts without the implementation of drastic public health interventions. Only absolute humidity might play a role.
14 October
Jefferies S, French N, Gilkison G, et al. COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. The Lancet 2020, published 13 October. Full-text: https://doi.org/10.1016/S2468-2667(20)30225-5
New Zealand’s government response resulted in low burden of disease, low levels of population disease disparities, and the initial achievement of COVID-19 elimination (Jefferies 2020, Robert 2020). Here, Sarah Jefferies et al. describe 1503 COVID-19 cases from Feb 2 to May 13, after which time community transmission ceased in New Zeeland, including 95 (6.3%) hospital admissions and 22 (1.5%) COVID-19 deaths. 1034 (69%) cases were imported or import related, tending to be younger adults, of European ethnicity, and of higher socioeconomic status. 702 (47%) cases were linked to 34 outbreaks.
See also the comment by Robert A. Lessons from New Zealand’s COVID-19 outbreak response. The Lancet 2020, published 13 October. Full-text: https://doi.org/10.1016/S2468-2667(20)30237-1
13 October
Soper GA. The lessons of the pandemic. Science 1919, published 30 May. Full-text: https://science.sciencemag.org/content/49/1274/501
Do some time travel.
10 October
Rader B, Scarpino SV, Nande A, et al. Crowding and the shape of COVID-19 epidemics. Nat Med 2020, published 5 October. Full-text: https://doi.org/10.1038/s41591-020-1104-0
The dynamic of the current SARS epidemics in Greater Paris and Madrid are reason for concern. In this article, Moritz Kraemer, Benjamin Rader and colleagues predict that crowded cities worldwide could experience more prolonged epidemics. The 2020/2021 autumn and winter season will be a hard time.
Oster AM, Caruso E, DeVies J, Hartnett KP, Boehmer TK. Transmission Dynamics by Age Group in COVID-19 Hotspot Counties — United States, April–September 2020. MMWR Morb Mortal Wkly Rep. ePub: 9 October 2020. Fulltext: http://dx.doi.org/10.15585/mmwr.mm6941e1
Understanding whether increasing incidence is predominantly occurring in specific age groups is important for identifying opportunities to prevent or reduce transmission. Here the authors analyze hotspot counties, particularly those in the US South and West. The positivity rate increased earliest in younger persons (18-24 years), followed by several weeks of increasing positivity among older age groups.
9 October
Rudberg A, Havervall S, Månberg A, et al. SARS-CoV-2 exposure, symptoms and seroprevalence in healthcare workers in Sweden. Nat Commun 11, 5064 (2020). https://doi.org/10.1038/s41467-020-18848-0
High transmission rate among Swedish healthcare workers. Among 2149 individuals recruited between April 14th and May 8th, the seroprevalence of IgG antibodies against SARS-CoV-2 was 19.1%. Seroprevalence was associated with patient contact (OR 2.9, 95% CI 1.9–4.5) and COVID-19 patient contact (OR 3.3, 95% CI 2.2–5.3). The majority of study participants were women (85%) and the mean age was 44 (SD 12) years. Fifty-three healthcare workers (13%) reported severe symptoms.
8 October
Editors. Dying in a Leadership Vacuum. N Engl J Med 2020; 383:1479-1480. Full-text: https://www.nejm.org/doi/full/10.1056/NEJMe2029812
SARS-CoV-2 and the COVID-19 pandemic became a test of leadership. With no good options to combat a novel pathogen, countries were forced to make hard choices about how to respond. In the United States, the leaders have failed that test.
7 October
Gallaway MS, Rigler J, Robinson S, et al. Trends in COVID-19 Incidence After Implementation of Mitigation Measures — Arizona, January 22–August 7, 2020. MMWR Morb Mortal Wkly Rep. ePub: 6 October 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6940e3
How community mitigation measures can help slow the spread of COVID-19. Case numbers in Arizona stabilized and then decreased after sustained implementation and enforcement of statewide and locally enhanced mitigation measures, beginning approximately 2 weeks after implementation and enforcement of mask mandates and enhanced sanitation practices began on June 17; further decreases were observed during July 13–August 7, after statewide limitations and closures of certain services and businesses.
Calcagno A, Ghisetti V, Emanuele T, et al. Risk of SARS-CoV-2 infection in healthcare workers, Turin, Italy. Emerg Infect Dis. 2021 Jan. Full-text: https://doi.org/10.3201/eid2701.203027
Among 5,444 healthcare workers in Italy, seroprevalence was 6.9%. Seroprevalence was highest in laboratory personnel (18/175, 10.3%), although numbers were small, followed by nurse assistants (44/520, 8.5%), nurses (150/1983, 7.6%), and doctors (55/755, 7.3%).
Vogel G. It’s been so, so surreal.’ Critics of Sweden’s lax pandemic policies face fierce backlash. Science October 6, 2020. Full-text: https://doi.org/10.1126/science.abf1247
Sweden’s approach to the coronavirus pandemic is out of step with much of the world. Until last month, Sweden’s official policy stated that people without obvious symptoms are very unlikely to spread the virus. Read how the Vetenskapsforum COVID-19 (Science Forum COVID-19) is fighting for tougher measures and how members have been pilloried or reprimanded.
6 October
Hicks SM, Pohl K, Neeman T, et al. A dual antigen ELISA allows the assessment of SARS-CoV-2 antibody seroprevalence in a low transmission setting. J Infect Dis. 2020 Oct 3:jiaa623. PubMed: https://pubmed.gov/33009908 . Full-text: https://doi.org/10.1093/infdis/jiaa623
There is low prevalence in Australia. Using an ELISA-based approach that combines IgG responses to both the Nucleocapsid and Spike-receptor binding domain antigens, the authors have shown that excellent sensitivity and specificity can be achieved in low prevalence areas. Frequency of antibodies in a cohort of 2,991 elective surgery patients providing blood samples at 10 hospital sites across Australia in June-July 2020 was only 0.28% (0 to 1.15%).
3 October
Boehmer TK, DeVies J, Caruso E, et al. Changing Age Distribution of the COVID-19 Pandemic — United States, May–August 2020. MMWR Morb Mortal Wkly Rep 2020;69:1404–1409. DOI: http://dx.doi.org/10.15585/mmwr.mm6939e1
First the kids, then the parents and, finally the grandparents (with unknown outcome)? During June–August 2020, SARS-CoV-2 incidence was highest in persons aged 20–29 years, who accounted for > 20% of all confirmed cases. Across the southern United States in June 2020, increases in percentage of positive SARS-CoV-2 test results among adults aged 20–39 years preceded increases among those aged ≥ 60 years by 4–15 days. The authors’ recommendations:
- Restrict in-person gatherings and events
- Recommend mask use and social distancing in settings where persons socialize
- Implement safe practices at on-site eating and drinking venues
- Enforce protection measures for essential and service industry workers
2 October
Buonanno P, Galletta S, Puca M, et al. Estimating the severity of COVID-19: Evidence from the Italian epicentre. PLOS October 1, 2020. Full-text: https://doi.org/10.1371/journal.pone.0239569
A tentative estimate of the number of deaths either directly or indirectly associated with COVID-19 as well as the total number of persons infected. The findings by Paola Buonanno and colleagues suggest that the reported number of deaths attributable to COVID-19 identified by public authorities accounts only for one half of the observed excess mortality between March 2020 and previous years.
1 October
Laxminarayan R, Dudala SR, Gopal K, et al. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science 30 Sep 2020: eabd7672. Full-text: https://doi.org/10.1126/science.abd7672
A detailed view into SARS-CoV-2 transmission pathways and mortality in India. Among 102,569 cases in Tamil Nadu and 22,315 cases in Andhra Pradesh who tested positive at least 30 days before the end of the study follow-up period, the overall case-fatality ratio was 2.06%. Reported cases and deaths have been concentrated in younger cohorts than expected from observations in higher-income countries, even after accounting for demographic differences across settings. Among 575,071 individuals exposed to 84,965 confirmed cases, infection probabilities ranged from 4.7-10.7% for low-risk and high-risk contact types. Same-age contacts were associated with the greatest infection risk.
30 September
Otte im Kampe E, Lehfeld AS, Buda Set al. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Euro Surveill 2020;25(38):pii=2001645. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.38.2001645
Only a few and mostly small COVID-19 school outbreaks have been reported in Germany overall. Since the start of the COVID-19 pandemic and until 31 August 2020, only 48 (0.5%) of documented 8,841 outbreaks in occurred in schools and included 216 cases, suggesting that containment measures in place are sufficient to reduce spillover into the community.
Wilson E, Donovan CV, Campbell M, et al. Multiple COVID-19 Clusters on a University Campus — North Carolina, August 2020. MMWR Morb Mortal Wkly Rep. ePub: 29 September 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6939e3
The campus may be another story. On August 3, 2020, a North Carolina university broadly opened campus for the first time since transitioning to primarily remote learning in March. Consistent with CDC guidance at that time, steps were taken to prevent the spread of SARS-CoV-2 on campus (daily symptom checks, use of masks in all indoor common spaces and classrooms, physical distancing of ≥ 6 feet in indoor and outdoor settings). These steps were not sufficient. Within 3 weeks, 670 laboratory-confirmed cases were identified; student gatherings and congregate living settings, both on and off campus, likely contributed to the rapid spread. Bad news for students.
28 September
Anand S, Montez-rath M, Han J, et al. Prevalence of SARS-CoV-2 antibodies in a large nationwide sample of patients on dialysis in the USA: a cross-sectional study. Lancet 2020, published 25 September. Full-text: https://doi.org/10.1016/S0140-6736(20)32009-2
During the first wave of the COVID-19 pandemic, fewer than 10% of the US adult population formed antibodies against SARS-CoV-2, and fewer than 10% of those with antibodies were diagnosed. That is the result of a cross-sectional US study by Shuchi Anand et al. after testing 28,503 randomly selected adult patients receiving dialysis in July 2020. When standardized to the US dialysis population, seroprevalence ranged from 3.5% in the west to 27.2% in the northeast. Residents of non-Hispanic Black and Hispanic neighborhoods experienced higher odds of seropositivity.
See also the comment by Barnaby Flower and Christina Atchison: Flower B, Atchison C. SARS-CoV-2 antibody seroprevalence in patients receiving dialysis in the USA. Lancet 2020, published 25 September. Full-text: https://doi.org/10.1016/S0140-6736(20)32006-7
Hallal PC, Hartwig FP, Horta BL, et al. SARS-CoV-2 antibody prevalence in Brazil: results from two successive nationwide serological household surveys. Lancet Global Health 2020, published 23 September. Full-text: https://doi.org/10.1016/S2214-109X(20)30387-9
A long way to herd immunity – and very different data from the projected 66% seropositivity rate in Manaus we presented two days ago. Cesar G Victora, Pedro Hallal and colleagues report two seroprevalence surveys in 133 sentinel cities in all Brazilian states. They included 25,025 participants in the first survey (May 14–21) and 31,165 in the second (June 4–7). Prevalence was strongly associated with Indigenous ancestry and low socioeconomic status. In the second survey, the authors observed an increased prevalence in participants aged 20–59 years and those living in crowded conditions (4.4% for those living with households with six or more people). Prevalence among Indigenous people was 6.4% compared with 1.4% among White people. Prevalence in the poorest socioeconomic quintile was 3.7% compared with 1.7% in the wealthiest quintile. The authors conclude that “these population subgroups are unlikely to be protected if the policy response to the pandemic by the national government continues to downplay scientific evidence.”
Gupta V, Bhoyar RC, Jain A, et al. Asymptomatic reinfection in two healthcare workers from India with genetically distinct SARS-CoV-2. Clin Infect Dis 2020, published 23 September. Full-text: https://doi.org/10.1093/cid/ciaa1451
The next paper on reinfection. Vinod Scaria, Vivek Gupta and colleagues describe two healthcare workers, 25 and 28 years old, who tested positive for SARS-CoV-2 in May and again, after resuming duties in the hospital, on 21 August and 5 September, respectively. Genomic analysis showed that the SARS-CoV-2 of the reinfection was different from the virus of the first episode. Both individuals were asymptomatic in May and in August/September.
26 September
Buss LF, Prete Jr CA, Abrahim CMM, et al. COVID-19 herd immunity in the Brazilian Amazon. medRxiv 2020, posted 21 September. Full-text: https://doi.org/10.1101/2020.09.16.20194787
As much as 66% of the population of Manaus (two million people), Brazil, could have been infected with SARS-CoV-2. Ester Sabino, Lewis Buss and colleagues show that the transmission of SARS-CoV-2 in Manaus increased quickly during March and April and declined slowly from May to September. In June, one month following the epidemic peak, 44% of the population was seropositive for SARS-CoV-2. After correcting for confounding factors, the authors estimate the epidemic size to be 66% by early August 2020. Note: these findings have not yet been peer reviewed.
Remember: herd immunity is defined as the proportion of a population that must be immune to an infectious disease, either by natural infection or vaccination, such that new cases decline and R0 falls below 1 (see also https://www.nature.com/articles/d41586-020-02009-w).
Boehmer TK, DeVies J, Caruso E, et al. Changing Age Distribution of the COVID-19 Pandemic — United States, May–August 2020. MMWR Morb Mortal Wkly Rep. ePub: 23 September 2020. DOI: http://dx.doi.org/10.15585/mmwr.mm6939e1
First the kids, then the parents and, finally, the grandparents. Tegan Boehmer et al. show that during June–August 2020, COVID-19 incidence was highest in persons aged 20–29 years. Across the southern United States in June 2020, increases in percentage of positive SARS-CoV-2 test results among adults aged 20–39 years preceded increases among those aged ≥ 60 years by 4–15 days. The authors conclude that preventive behavior by younger adults is needed to help reduce infection and subsequent transmission to persons at higher risk for severe illness.
25 September
Briefing. The covid-19 pandemic is worse than official figures show. The Economist 2020, published 26 September. Full-text: https://www.economist.com/briefing/2020/09/26/the-covid-19-pandemic-is-worse-than-official-figures-show
“As the autumnal equinox passed, Europe was battening down the hatches for a gruelling winter. Intensive-care wards and hospital beds were filling up in Madrid and Marseille—a city which, a few months ago, thought it had more or less eliminated covid-19. Governments were implementing new restrictions, sometimes, as in England, going back on changes made just a few months ago. The al-fresco life of summer was returning indoors. Talk of a second wave was everywhere.”
24 September
Brett TS, Rohani P. Transmission dynamics reveal the impracticality of COVID-19 herd immunity strategies. Proc Natl Acad Sci U S A. 2020 Sep 22:202008087. PubMed: https://pubmed.gov/32963094. Full-text: https://doi.org/10.1073/pnas.2008087117
Various governments have entertained the idea of achieving herd immunity through natural infection as a means of ending the long-term threat of COVID-19. This has provoked alarm in sections of the public health community. This work confirms that this alarm is well-founded: if social distancing is maintained at a fixed level, hospital capacity needs to be much larger than presently available to achieve herd immunity without exceeding capacity; otherwise, the final outbreak size will be insufficient to achieve herd immunity.
23 September
Lash RR, Donovan CV, Fleischauer AT, et al. COVID-19 Contact Tracing in Two Counties — North Carolina, June–July 2020. MMWR Morb Mortal Wkly Rep. ePub: 22 September 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6938e3
Despite aggressive efforts by health departments, many COVID-19 patients do not report contacts, and many contacts cannot be reached. Staff members in North Carolina, US have investigated 5514 (77%) persons with COVID-19 in Mecklenburg County and 584 (99%) in Randolph County: during periods of high COVID-19 incidence, 48% and 35% of patients reported no contacts, and 25% and 48% of contacts were not reached. Median interval from index patient specimen collection to contact notification was 6 days. Improved timeliness of contact tracing, community engagement, and community-wide mitigation are needed to reduce SARS-CoV-2 transmission.
22 September
Mecenas P, Bastos RTDRM, Vallinoto ACR, Normando D. Effects of temperature and humidity on the spread of COVID-19: A systematic review. PLoS One. 2020 Sep 18;15(9):e0238339. PubMed: https://pubmed.gov/32946453. Full-text: https://doi.org/10.1371/journal.pone.0238339
Don’t count on the weather. This systematic review of seventeen studies found that cold and dry conditions were potentiating factors on the spread of the virus. Warm and wet climates seem to reduce the spread of COVID-19. However, these variables alone could not explain most of the variability in disease transmission. Therefore, the countries most affected by the disease should focus on health policies, even those with climates less favorable to the virus.
19 September
Ruktanonchai NW, Floyd JR, Lai S, et al. Assessing the impact of coordinated COVID-19 exit strategies across Europe. Science 2020, published 18 September. Full-text: https://doi.org/10.1126/science.abc5096
Ruktanonchai et al. used mobility data from smartphones to estimate movements between administrative units across Europe before and after the implementation of NPIs (non-pharmaceutical interventions) for COVID-19. The result: if countries do not coordinate their NPIs when they relax lockdown, resurgence of disease occurs faster. Remember: collaboration is better than unilateralism. Some people should have thought about that before voting Brexit.
17 September
Ng DL, Goldgof GM, Shy BR, et al. SARS-CoV-2 seroprevalence and neutralizing activity in donor and patient blood. Nat Commun 11, 4698 (2020). https://doi.org/10.1038/s41467-020-18468-8
In April 2020, SARS-CoV-2 seroprevalence was low in the San Francisco Bay Area (0.26% in 387 hospitalized patients; 0.1% in 1,000 blood donors). Charles Y. Chiu, Dianna Ng and colleagues also describe the longitudinal dynamics of immunoglobulin-G (IgG), immunoglobulin-M (IgM), and in vitro neutralizing antibody titers in COVID-19 patients. The median time to seroconversion ranged from 10.3–11.0 days for these 3 assays. The authors provide evidence that seropositive results using SARS-CoV-2 anti-nucleocapsid protein IgG and anti-spike IgM assays are generally predictive of in vitro neutralizing capacity.
16 September
Kissle SM, Kishore N, Prabhu M, et al. Reductions in commuting mobility correlate with geographic differences in SARS-CoV-2 prevalence in New York City. Nat Commun 11, 4674 (2020). Full-text: https://doi.org/10.1038/s41467-020-18271-5
SARS-CoV-2 prevalence varied substantially between New York City boroughs between 22 March and 3 May 2020 (for example, Manhattan: 11.3%; South Queens: 26.0%). These differences in prevalence correlate with antecedent reductions in commuting-style mobility between the boroughs. Prevalence was lowest in boroughs with the greatest reductions in morning movements out of and evening movements into the borough.
Rogers JH, Link AC, McCulloch D, et al. Characteristics of COVID-19 in Homeless Shelters. Ann Intern Med 2020, published 15 September. Full-text: https://doi.org/10.7326/M20-3799
In this cross-sectional, community-based surveillance study of 14 homeless shelters in King County, Washington, Helen Chu, Julia Rogers and colleagues divided the number of positive cases by the total number of participant encounters, regardless of symptoms. Among 1434 encounters, 29 (2%) cases of SARS-CoV-2 infection were detected across 5 shelters. Eighty-six percent of persons with positive test results slept in a communal space rather than in a private or shared room.
13 September
Thomas LJ, Hunag O, Yin F, et al. Spatial heterogeneity can lead to substantial local variations in COVID-19 timing and severity. PNAS September 10, 2020. Full-text: https://doi.org/10.1073/pnas.2011656117
Loring J. Thomas and colleagues examined the potential impact of local spatial heterogeneity on COVID-19, modelling the diffusion of SARS-CoV-2 in populations whose contacts are based on spatially plausible network structures. They focus here on the urban context, examining 19 different cities in the US. The main results: The spread of COVID-19 is much “burstier” than in standard epidemiological models, with substantial local disparities in timing and severity and long lags between local outbreaks. Spatial heterogeneity may produce dramatic differences in social exposures to those with the illness, and may stress health care delivery systems in ways that are not well captured by standard models.
11 September
Worobey M, Pekar J, Larsen BB, et al. The emergence of SARS-CoV-2 in Europe and North America. Science 2020, published 10 September. Full-text: https://doi.org/10.1126/science.abc8169
The first early interventions successfully prevented early introduction of the virus into Germany and the US. But subsequent introductions found sustained European and North America transmission networks during the first two months of 2020: first in Italy around the end of January, then in Washington State around the beginning of February, followed by New York City later that month. Here, Philippe Lemey, Michael Worobey delineate when widespread community transmission was first established on both continents (see Figure 6) and clarify the period before SARS-CoV-2 establishment when contact tracing and isolation might have been most effective. Delaying COVID-19 outbreaks by even a few weeks in the US and Europe (the public health response to the WA1 case in Washington State, and a particularly impressive response in Germany to an early outbreak), bought crucial time for their own cities, as well as other countries and cities, to prepare for the virus when it finally did arrive. Don’t miss this paper.
9 September
Gandhi M, Rutherford GW. Facial Masking for Covid-19 — Potential for “Variolation” as We Await a Vaccine. NEJM September 8, 2020. Full-text: https://doi.org/10.1056/NEJMp2026913
In this perspective, Monica Gandhi and George W. Rutherford review the growing evidence that universal facial masking might help reduce the severity of disease and ensure that a greater proportion of new infections are asymptomatic. If this hypothesis is borne out, universal masking could become a form of “variolation” (inoculation) that would generate immunity and thereby slow the spread of the virus.
7 September
Khan A, Bieh KL, El-Ganainy A, et al. Estimating the COVID-19 Risk during the Hajj Pilgrimage. Journal of Travel Medicine, 05 September 2020. Full-text: https://doi.org/10.1093/jtm/taaa157
The Hajj, which is held in Makkah, Kingdom of Saudi Arabia (KSA), attracts around 2.5 million Muslim pilgrims from over 150 countries annually. Based on risk estimates, the Ministry of Hajj and Umra announced a reduction in the number of pilgrims and the exclusion of foreign pilgrims from the 2020 Hajj. This was probably a wise decision: The authors calculate that the existing number of designated ward and ICU beds in the Hajj areas would be saturated once the total Hajj population exceeds around 10-15% of the previous five years’ average.
Nayar KR, Koya SF, Ramakrishnan V, et al. Call to avert acceleration of COVID-19 from India’s Sabarimala pilgrimage of 25 million devotees. Journal of Travel Medicine, 05 September 2020, taaa153. Full-text: https://doi.org/10.1093/jtm/taaa153
The next problem. The forthcoming Sabarimala annual Hindu pilgrimage of 41 days duration normally held during the months of November to December at the Sabarimala peak in India is attended by (yes, you’re reading correctly) an average of 25 million pilgrims. Currently, for routine non-mass gathering visits to Sabarimala, the State Government requires all pilgrims to submit a negative SARS-CoV-2 antigen test result through the online queue system. But this may be impractical and insufficient when 25 million devotees or more congregate during the annual pilgrimage. Unlike the Hajj pilgrimage (see above) which is international, the quota is based on and restricted through a visa process, participation in Sabarimala pilgrimage, a domestic event, is uncoordinated and required no registration for participation until last year. The authors discuss the options.
Moreland A, Herlihy C, Tynan MA, et al. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement – United States, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020 Sep 4;69(35):1198-1203. PubMed: https://pubmed.gov/32881851 . Full-text: https://doi.org/10.15585/mmwr.mm6935a2
People are compliant to mandatory stay-at-home orders. Based on location data from mobile devices, in 97.6% of counties these orders were associated with decreased median population movement after the order start date, relative to the period before the order was implemented.
6 September
Barbarossa MV, Fuhrmann J, Meinke JH, et al. Modeling the spread of COVID-19 in Germany: Early assessment and possible scenarios. PLoS One. 2020 Sep 4;15(9):e0238559. PubMed: https://pubmed.gov/32886696. Full-text: https://doi.org/10.1371/journal.pone.0238559
Maria Vittoria Barbarossa and colleagues have used complex mathematical models to reproduce data of the early evolution of the COVID-19 outbreak in Germany, taking into account the effect of actual and hypothetical non-pharmaceutical interventions. Interesting finding: a partial (and gradual) lifting of introduced control measures could soon be possible if accompanied by further increased testing activity, strict isolation of detected cases, and reduced contact to risk groups. However, in scenarios without appropriate measures, simulations predict incredibly high peaks in active cases and alarmingly high numbers of deaths far into the future. If no restrictive measures and interventions were to be (re)introduced, the simulation of the model results in about 32 million total infections and 730,000 deaths over the course of the epidemic, which seems to occur only by the end of the summer 2021 under the assumption that no reliable treatment becomes available before then. Just saying.
Marossy A, Rakowicz S, Bhan A, et al. A study of universal SARS-CoV-2 RNA testing of residents and staff in a large group of care homes in South London. J Infect Dis. 2020 Sep 5:jiaa565. PubMed: https://pubmed.gov/32889532. Full-text: https://doi.org/10.1093/infdis/jiaa565
One of the largest studies of care homes in Europe, involving 2,455 individuals tested irrespective of symptoms. Combined nose and throat swab testing for SARS-CoV-2 RNA was carried out in residents and staff across 37 care homes in the London Borough of Bromley across a three-week period. Overall, the point prevalence of SARS-CoV-2 infection was 6.5% with a higher rate in residents (9.0%) than in staff (4.7%). A key finding was the high proportion of asymptomatic infection detected in staff (69%) and residents (51%) with evidence of under-detection of symptoms by care home staff.
4 September
Lordan R, FitzGerald GA, Grosser T. Reopening schools during COVID-19. Science 04 Sep 2020: Vol. 369, Issue 6508, pp. 1146. Full-text: https://doi.org/10.1126/science.abe5765
A note from daily practice. On Thursday, September 3, at our infectious disease clinic in Hamburg, Germany, we found a young male teacher (under 40 years old) to be PCR positive. For the previous three days, he had given lectures to at least 12 classes, despite having (mild) symptoms. How to avoid, how to deal with this situation? This editorial gives some answers, recommending different mitigation strategies for the re-opening of schools.
The national COVID-19 outbreak monitoring group. COVID-19 outbreaks in a transmission control scenario: challenges posed by social and leisure activities, and for workers in vulnerable conditions, Spain, early summer 2020. Eurosurveillance Volume 25, Issue 35, 03/Sep/2020. Full-text: https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.35.2001545
From mid-June to 2 August, excluding single household outbreaks, 673 outbreaks were notified in Spain. There were two main settings where over 55% of active outbreaks (303/551) and over 60% (3,815/6,208) of active outbreak cases originated: First, social settings such as family gatherings or private parties (112 outbreaks, 854 cases), followed by those linked to leisure venues such as bars, restaurants, or clubs (34 outbreaks, over 1,230 cases). Second, occupational settings (representing 20% of all active outbreaks), mainly among workers in the fruit and vegetable sector (31 outbreaks and around 500 cases) and workers at slaughterhouses or meat processing plants (12 outbreaks and around 360 cases).
3 September
Self WH, Tenforde MW, Stubblefield WB, et al. Seroprevalence of SARS-CoV-2 Among Frontline Health Care Personnel in a Multistate Hospital Network — 13 Academic Medical Centers, April–June 2020. MMWR. Full-text: http://dx.doi.org/10.15585/mmwr.mm6935e2
Many appear to go undetected: among 3,248 HCWs who routinely cared for COVID-19 patients in 13 US academic medical centers from February 1, 2020, 194 (6%) had evidence of previous SARS-CoV-2 infection, with considerable variation by location that generally correlated with community cumulative incidence. Among 194 participants who had SARS-CoV-2 antibodies, 56 (29%) did not recall any symptoms consistent with an acute viral illness in the preceding months and 133 (69%) did not have a previous positive test result demonstrating an acute SARS-CoV-2 infection. Prevalence of SARS-CoV-2 antibodies was lower among personnel who reported always wearing a face covering while caring for patients (6%), compared with those who did not (9%).
1 September
Seemann T, Lance CR, Sherry NL, et al. Tracking the COVID-19 pandemic in Australia using genomics. Nat Commun 11, 4376 (2020). Full-text: https://doi.org/10.1038/s41467-020-18314-x
Genomic sequencing for rapid identification of SARS-CoV-2 transmission chains? That’s what Benjamin P. Howden and Torsten Seemann did in Victoria, Australia (1,333 COVID-19 cases). They combined extensive whole-genome sequencing and epidemiologic data to investigate the source of individual cases and identify distinct genomic clusters, including large clusters associated with social venues, healthcare visits and cruise ships. The authors demonstrate the critical role of multiple SARS-CoV-2 importations by returned international travelers in driving transmission in Australia, with travel-related cases responsible for establishing ongoing transmission lineages (each with 3–9 cases) accounting for over half of locally acquired cases.
31 August
Westhaus S, Weber FA, Schiwy S, et al. Detection of SARS-CoV-2 in raw and treated wastewater in Germany – Suitability for COVID-19 surveillance and potential transmission risks. Sci Total Environ 2020 August 18;751:141750. PubMed: https://pubmed.gov/32861187. Full-text: https://doi.org/10.1016/j.scitotenv.2020.141750
Detailed Analysis of a set of samples from nine wastewater treatment plants in North Rhine-Westphalia, Germany. Main conclusions: Yes, SARS-CoV-2 can be detected in wastewater in Germany using RT-qPCR. The total load of gene equivalents in wastewater correlated with the cumulative and the acute number of COVID-19 cases reported in the respective catchment areas. Thus, wastewater-based epidemiology can be regarded as a complementary measure to survey the outbreak. Note – negative tests for replication potential indicate that wastewater might be no major route for transmission to humans.
Graham NSN, Junghans C, McLaren R, et al. High rates of SARS-CoV-2 seropositivity in nursing home residents. J Infection August 26, 2020. Full-text: https://doi.org/10.1016/j.jinf.2020.08.040
What incredibly high infection rates in nursing homes! During March – April 2020 the authors investigated outbreaks in four UK nursing homes where 40% of 394 residents tested positive on RT-PCR. Now they demonstrate that COVID-19 infection was considerably more widespread. Seventy-two percent of nursing home residents (95% CI 66 – 77) were anti-SARS-CoV-2 IgG antibody positive, representing 173 of 241 residents available and consenting to testing. This included 93% of those tested who were previously RT-PCR positive and 59% of those who were previously RT-PCR negative. Seropositivity was not associated with the presence of comorbidities.
Fouillet A, Pontais I, Caserio-Schönemann C. Excess all-cause mortality during the first wave of the COVID-19 epidemic in France, March to May 2020. Eurosurveillance 2020;25(34. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.34.2001485
Through a weekly all-cause mortality surveillance system in France, the authors observed a major all-cause excess mortality from March to May 2020 (25,030 deaths, mainly among elderly people). Five metropolitan regions were the most affected, particularly the Île-de-France and the Grand-Est regions. However, assessing the excess mortality related to COVID-19 is complex because of the potential protective effect of the lockdown period on other causes of mortality.
27 August
Maxmen A. Why the United States is having a coronavirus data crisis. Nature 2020, published 25 August. Full-text: https://www.nature.com/articles/d41586-020-02478-z
Is the United States emerging as a Second-World country from the SARS-CoV-2 pandemic? The country suffers from a dearth of data, writes Amy Maxmen in this Nature news article. Reliable information on who is infected, why and where is simply missing. How could this happen?
26 August
Perkins TA, Cavany SM, Moore SM, et al. Estimating unobserved SARS-CoV-2 infections in the United States. PNAS August 21, 2020. Full-text: https://doi.org/10.1073/pnas.2005476117
The authors quantified unobserved infections in the United States during the early weeks of the epidemic. After a national emergency was declared, fewer than 10% of locally acquired, symptomatic infections in the US were detected over a period of a month. This gap in surveillance during a critical phase of the epidemic resulted in a large, unobserved reservoir by early March. Testing was a major limiting factor in assessing the extent of SARS-CoV-2 transmission during its initial invasion into the US.
22 August
Hatcher SM, Agnew-Brune C, Anderson M, et al. COVID-19 Among American Indian and Alaska Native Persons — 23 States, January 31–July 3, 2020. MMWR Morb Mortal Wkly Rep 2020, published 19 August 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6934e1
American Indian and Alaska Native (AI/AN) persons appear to be disproportionately affected by the COVID-19 pandemic. Now Sarah Hatcher et al. report that the overall COVID-19 incidence among AI/AN persons was 3.5 times that among white persons (594 per 100,000 AI/AN population compared with 169 per 100,000 white population). The authors discuss the factors which most likely contributed to the observed elevated incidence.
Jiménez MC, Cowger TL, Simon LE, Behn M, Cassarino N, Bassett MT. Epidemiology of COVID-19 Among Incarcerated Individuals and Staff in Massachusetts Jails and Prisons. JAMA Netw Open 2020;3(8). Full-text: https://doi.org/10.1001/jamanetworkopen.2020.18851
Of 14,987 individuals incarcerated across Massachusetts prison facilities, 1032 confirmed cases of COVID-19 were reported among incarcerated individuals (n = 664) and staff (n = 368) as of July 8, 2020. The rate of COVID-19 among incarcerated individuals was nearly 3 times that of the Massachusetts general population and 5 times the US rate. Monik Jiménez et al. stress that access to testing without coercion, de-carceration, and contact tracing are necessary to decrease harm from COVID-19 to incarcerated people and their communities.
20 August
Rivera F, Safdar N, Ledeboer N, et al. Prevalence of SARS-CoV-2 asymptomatic infections in two large academic health systems in Wisconsin. Clinical Infectious Diseases 19 August 2020. Full-text: https://doi.org/10.1093/cid/ciaa1225
From April 6 2020 to June 4 2020, a total of 11,654 asymptomatic patients were tested for SARS-CoV-2 in two large academic health systems in two counties of Wisconsin. Since early April 2020, both health systems implemented SARS-CoV-2 testing on all hospitalizations, on all patients scheduled for elective surgeries, including deliveries, or among all patients with known SARS-CoV-2 exposure in the absence of symptoms. In total, only 61 (0.52%) were positive. In both of these counties, rates were low, despite the higher incidence of COVID-19 in Milwaukee county.
16 August
Sebhatu A, Wennberg K, Arora-Jonsson S, et al. Explaining the homogeneous diffusion of COVID-19 nonpharmaceutical interventions across heterogeneous countries. PNAS August 11, 2020. Full-text: https://doi.org/10.1073/pnas.2010625117
What drives OECD countries to adopt COVID-19 restrictive policies such as lockdowns and school closures? These Swedish researchers found that government policies are strongly driven by the policies initiated in other countries. The level of democracy also matters: While strong democracies are slower to initiate restrictive policies, they are more likely to follow the policies of nearby countries. Following the lead of others rather than making decisions based on the specific situation of the country may have led to countries locking down too early or too late.
14 August
Ward H, Atchison C, Whitaker M, et al. Antibody prevalence for SARS-CoV-2 following the peak of the pandemic in England: REACT2 study in 100,000 adults. Imperial College London 2020. Pre-print: https://www.imperial.ac.uk/media/imperial-college/institute-of-global-health-innovation/Ward-et-al-120820.pdf
By the end of June, an estimated 3.4 million people, or slightly under 6% of the UK population, had antibodies to the virus and had likely had COVID-19. London had the highest numbers (13%), while the South West had the lowest (3%). This is the result of the REACT (REal Time Assessment of Community Transmission) study, by Helen Ward, Paul Elliott and colleagues from the Imperial College London, using antibody finger-prick self-testing at home to track past infections. Black, Asian and minority ethnic (BAME) individuals were between two and three times as likely to have had SARS-CoV-2 infection compared to white people. An interesting trend: young people aged 18-24 had the highest rates (8%), while older adults aged 65 to 74 were least likely to have been infected (3%).
13 August
Steinberg J, Kennedy ED, Basler C, et al. COVID-19 Outbreak Among Employees at a Meat Processing Facility — South Dakota, March–April 2020. MMWR Morb Mortal Wkly Rep 2020;69:1015–1019. Full-text: http://dx.doi.org/10.15585/mmwr.mm6931a2
Detailed report of an outbreak in a meat processing facility in South Dakota. From March 16 to April 25, 25.6% (929) of employees and 8.7% (210) of their contacts were diagnosed with COVID-19; two employees died. The highest attack rates occurred among employees who worked < 6 feet (2 meters) from one another on the production line.
10 August
Kalk A, Schultz A. SARS-CoV-2 epidemic in African countries—are we losing perspective? Lancet, August 07, 2020. Full-text: https://doi.org/10.1016/S1473-3099(20)30563-6
Important comment on modelling studies predicting a huge death toll for some African countries. In the Democratic Republic of the Congo and Malawi, for instance, only 2-3% of the population is older than 65 years. According to the two authors (who work in these countries), the lockdown measures proposed by others do not appear applicable to the African continent and might cause more harm than SARS-CoV-2 itself.
9 August
Baker MG, Anglemyer A. Successful Elimination of Covid-19 Transmission in New Zealand. N Engl J Med 2020, published 7 August. Full-text: https://www.nejm.org/doi/full/10.1056/NEJMc2025203
In mid-March, informed by science-based advocacy, national New Zealand leaders switched from a mitigation strategy to an elimination strategy. The government implemented a stringent countrywide lockdown which lasted 7 weeks (26 March – mid-May). Now, New Zealand views itself in the post-elimination stage, and public life has returned to near normal. The only cases identified are among international travelers who are kept in government-managed quarantine or isolation for 14 days after arrival. Michael Baker and Andrew Anglemyer conclude that rapid, science-based risk assessment linked to early, decisive government action was critical. The geographical isolation of New Zealand was another trump card the country had up its sleeve.
Heywood AE, Macintyre CR. Elimination of COVID-19: what would it look like and is it possible? Lancet 2020, published 6 August. Full-text: https://doi.org/10.1016/S1473-3099(20)30633-2
Anita Haywood and Raina Macintyre remember that the elimination of any infectious disease is ambitious, requiring substantial resources. They suggest a zero-case scenario of not less than three months before declaring an area SARS-CoV-2-free. For obvious reasons, islands or island states have the best chances to achieve this goal.
Moscola J, Sembajwe G, Jarrett M, et al. Prevalence of SARS-CoV-2 Antibodies in Health Care Personnel in the New York City Area. JAMA 2020, published 6 August. https://doi.org/10.1001/jama.2020.14765
Health care personnel (HCP) working in New York City had a high exposure risk for SARS-CoV-2 infection. To address this concern, the Northwell Health System, the largest in New York State, offered voluntary antibody testing to all HCPs. Now Karina Davidson and colleagues report the prevalence of SARS-CoV-2 among HCPs and associations with demographics, primary work location and type, and suspicion of viral exposure. They found a 13.7% prevalence of SARS-CoV-2 antibodies (5523 of 40,329 HCWs tested) which was similar to that among adults randomly tested in New York State (14.0%).
Petersen MS, Strøm M, Christiansen DH, Fjallsbak JP, Eliasen EH, Johansen M, et al. Seroprevalence of SARS-CoV-2–specific antibodies, Faroe Islands. Emerg Infect Dis 2020 Nov. Published August 2020. Full-text: https://doi.org/10.3201/eid2611.202736
Maria Petersen and colleagues conducted a nationwide study of the prevalence of SARS-CoV-2 infection in the Faroe Islands, an autonomous territory within the Kingdom of Denmark with a population of around 50,000. Of 1,075 randomly selected participants, 6 (0.6%) tested seropositive for antibodies to the virus. At present, small islands tend to have low seropositivity rates.
7 August
To KK, Chan WM, Ip JD, et al. Unique SARS-CoV-2 clusters causing a large COVID-19 outbreak in Hong Kong. Clin Infect Dis. 2020 Aug 5:ciaa1119. PubMed: https://pubmed.gov/32756996. Full-text: https://doi.org/10.1093/cid/ciaa1119
With a total of 617 locally acquired laboratory-confirmed cases reported between July 5 and 21, Hong Kong has experienced the largest local COVID-19 outbreak since the beginning of the pandemic. This phylogenetic study by Kwok-Yung Yuen, Kelvin Kai-Wang To and colleagues shows that this outbreak was related to imported cases and not to silent carriers from previous waves. Two unique SARS-CoV-2 clusters were identified.
16 July
Islam N, Sharp SJ, Chowell G, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. 2020 Jul 15;370:m2743. PubMed: https://pubmed.gov/32669358. Full-text: https://doi.org/10.1136/bmj.m2743
Be fast – but don’t close the metro. In this large empirical study, data from 149 countries were pooled, in order to estimate the relative effectiveness of different policy interventions within each country. Implementation of any physical distancing intervention was associated with an overall incidence reduction of 13% (IRR 0.87). Closure of public transport was not associated with any additional reduction when the other four physical distancing interventions were in place. Data from 11 countries also suggested similar overall effectiveness (IRR 0.85) when school closures, workplace closures, and restrictions on mass gatherings were in place. Earlier implementation of lockdown was associated with a larger reduction (IRR 0.86) compared with a delayed implementation of lockdown after other physical distancing interventions were in place (IRR 0.90).
14 July
Rincón A, Moreso F, López-Herradón A. The keys to control a coronavirus disease 2019 outbreak in a haemodialysis unit. Clinical Kidney Journal, 13 July 2020. Full-text: https://doi.org/10.1093/ckj/sfaa119
Outbreak in an hemodialysis unit in Barcelona, involving 18% of patients receiving treatment in this facility. In total, 22 symptomatic and 14 of the 170 asymptomatic patients became infected. The main risk factors for SARS-CoV-2 infection were sharing health-care transportation, living in a nursing home and having been admitted to the reference hospital within the previous 2 weeks.
12 July
Verdery AM, Smith-Greenaway E, Margolis R, Daw J. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc Natl Acad Sci U S A. 2020 Jul 10:202007476. PubMed: https://pubmed.gov/32651279. Full-text: https://doi.org/10.1073/pnas.2007476117
Multiply deaths by nine. These authors created a “bereavement multiplier”, an indicator that clarifies the downstream impact of COVID-19 mortality and can be applied to different epidemiological projections of death counts: how many people are at risk for losing a grandparent, parent, sibling, spouse, or child for each COVID-19 death. In the US, every death from COVID-19 will leave approximately nine bereaved.
Fenton MB. Bats navigate with cognitive maps. Science 10 Jul 2020: Vol. 369, Issue 6500, pp. 142. Full-text: https://doi.org/10.1126/science.abd1213
Interested in bats these days? They are smart. And they know where they are. This article summarizes current research on the path-finding strategies of fruit bats. Bats do not systematically follow known routes, nor do they directly sense cues such as landmarks or beacons: they rely on a cognitive map frame of reference for their current positions in relation to a goal that they had not yet detected.
11 July
Torres JP, Piñera C, De La Maza V, et al. SARS-CoV-2 antibody prevalence in blood in a large school community subject to a Covid-19 outbreak: a cross-sectional study. Clin Infect Dis. 2020 Jul 10:ciaa955. PubMed: https://pubmed.gov/32649743. Full-text: https://doi.org/10.1093/cid/ciaa955
In this school-based outbreak in Santiago, Chile identified on March 12, affecting nearly 50 people among school and household members, antibody positivity rates based on a self-administered test were 9.9% for 1,009 students and 16.6% for 235 staff. Among students, positivity was associated with younger age (p = 0.01), lower grade level (p = 0.05), prior RT-PCR positivity (p = 0.03), and history of contact with a confirmed case (p < 0.001). Among staff, positivity was higher in teachers (p = 0.01) and in those previously RT-PCR positive (p < 0.001). Teachers were more affected during the outbreak and younger children were at higher infection risk, likely because index case(s) were teachers and/or parents from preschool. Reopening schools should focus on avoiding new cases among teachers.
10 July
Houlihan CF, Vora N, Byrne T, et al. Pandemic peak SARS-CoV-2 infection and seroconversion rates in London frontline health-care workers. Lancet July 09, 2020. Full-text: https://doi.org/10.1016/S0140-6736(20)31484-7
A total of 200 high-risk frontline HCWs were enrolled between March 26 and April 8 in a prospective cohort study in an acute National Health Service hospital trust in London. 25% of HCWs were already seropositive at enrolment and a further 20% became seropositive within the first month of follow-up. Most infections occurred between March 30 and April 5, the week with the highest number of new cases in London.
The Lancet. COVID-19: the worst may be yet to come. Lancet July 11, 2020. Full-text: https://doi.org/10.1016/S0140-6736(20)31517-8
What a depressing editorial. Don’t read this if you’re in a bad mood. Five months after WHO declared the SARS-CoV-2 outbreak a global health emergency, the virus continues to beat a concerning and complex path. For much of the globe, the worst may be yet to come.
Watsa M. Rigorous wildlife disease surveillance. Science 10 Jul 2020, 369: 145-147. Full-text: https://doi.org/10.1126/science.abc0017
There are no international or national conventions on pathogen screening associated with animals, animal products or their movements. Capacity for emerging infectious disease (EID) diagnostics is limited along much of the human-wildlife interface. EID risks associated with the wildlife trade remain the largest unmet challenge of current disease surveillance efforts. According to this comment, an internationally recognized standard for managing wildlife trade on the basis of known disease risks should be established.
9 July
Saloner B, Parish K, Ward JA. COVID-19 Cases and Deaths in Federal and State Prisons. JAMA July 8, 2020. Full-text: https://doi.org/10.1001/jama.2020.12528
By June 6, 2020, there had been 42,107 cases of COVID-19 and 510 deaths among 1.3 million prisoners in the US. The case rate was initially lower in prisons but surpassed the US population on April 14, 2020. The mean daily case growth rate was 8.3% per day in prisons and 3.4% per day in the US population.
Maxmen A. California’s San Quentin prison declined free coronavirus tests and urgent advice — now it has a massive outbreak. Nature NEWS 07 July 2020. Full-text: https://doi.org/10.1038/d41586-020-02042-9
And this is a story behind the numbers. San Quentin Prison, which got through most of May without a single reported case among inmates, is now dealing with the third-largest coronavirus outbreak in the US. More than one-third of the inmates and staff (1,600 people) have tested positive. Six have died. Researchers fear that other institutions are at risk.
8 July
Kang CR, Lee JY, Park Y, Huh IS, Ham HJ, Han JK, et al. Coronavirus disease exposure and spread from nightclubs, South Korea. Emerg Infect Dis. 2020 Sep. Full-text: https://doi.org/10.3201/eid2610.202573 l (Important)
Despite low incidence, superspreading related to visiting nightclubs has the potential to spark a resurgence of cases. This article describes large-scale testing for active case-finding among persons who visited 5 Itaewon nightclubs in downtown Seoul, South Korea. Nightclubs had reopened ahead of the April 30–May 5 Golden Week holiday. Among the 41,612 total tests (!) conducted by May 25, positive results were found in 0.19% (67/35,827) of nightclub visitors, 0.88% (51/5,785) of their contacts, and 0.06% (1/1,627) of anonymously tested persons. 246 COVID-19 cases were associated with the reopening of nightclubs in Seoul. Hooray for the Asian thoroughness and some strong arguments against reopening nightclubs…
Yehya N, Venkataramani A, Harhay MO. Statewide Interventions and Covid-19 Mortality in the United States: An Observational Study. Clin Infect Dis. 2020 Jul 8. PubMed: https://pubmed.gov/32634828. Full-text: https://doi.org/10.1093/cid/ciaa923
Every day counts. In this large, nationwide study, later statewide emergency declarations and school closures were associated with higher COVID-19 mortality. Each day of delay increased mortality risk by 5 to 6%.
Waltenburg MA, Victoroff T, Rose CE, et al. Update: COVID-19 Among Workers in Meat and Poultry Processing Facilities – United States, April–May 2020. MMWR Morb Mortal Wkly Rep. ePub: 7 July 2020. Full-text: https://www.cdc.gov/mmwr/volumes/69/wr/mm6927e2.htm
One more reason to go veg. Overall, 239 facilities reported 16,233 COVID-19 cases and 86 COVID-19–related deaths among workers. The percentage of workers with COVID-19 ranged from 3.1% to 24.5% per facility. Among seven facilities that implemented facility-wide testing, the crude prevalence of asymptomatic or presymptomatic infections among 5,572 workers who had positive SARS-CoV-2 test results was 14.4%.
6 July
Adam D. A guide to R — the pandemic’s misunderstood metric. Nature News. 03 July 2020. Full-text: https://www.nature.com/articles/d41586-020-02009-w
Nice article about what R, the reproduction number, can and can’t tell us about managing COVID-19. Politicians seem to have embraced R with enthusiasm but it’s far more important to watch for clusters of cases and to set up comprehensive systems to test people, trace their contacts and isolate those infected, than to look at R.
Pollán M, Pérez-Gómez B, Pastor-Barriuso R, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. The Lancet 2020, July 06, 2020. Full-text: https://doi.org/10.1016/S0140-6736(20)31483-5
The vast majority (95%) of the Spanish population is seronegative, even in hotspot areas. In this nationwide, representative study, 61,075 participants were tested. Seroprevalence was 5·0% (95% CI 4.7–5.4) by the point-of-care test and 4.6% (4.3–5.0) by immunoassay, with a lower seroprevalence in children younger than 10 years (< 3.1% by the point-of-care test). There was high geographical variability, with higher prevalence around Madrid (> 10%) and lower in coastal areas (< 3%).
Eckerle I, Meyer B. SARS-CoV-2 seroprevalence in COVID-19 hotspots. The Lancet July 06, 2020. Full-text: https://doi.org/10.1016/S0140-6736(20)31482-3
Comment on these findings. Most of the population appears to have remained unexposed to SARS-CoV-2, even in areas with widespread virus circulation. Any proposed approach to achieve herd immunity through natural infection is not only highly unethical, but also unachievable. With a large majority of the population being infection-naïve, virus circulation can quickly return to early pandemic dimensions in a second wave once measures are lifted.
5 July
Petersen E, Koopmans M, Go U, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Inf Dis 2020, July 03, 2020. Full-text: https://doi.org/10.1016/S1473-3099(20)30484-9
The basic reproductive rate (R0) for SARS-CoV-2 is estimated to be 2·5 (range 1·8–3·6) compared with 2·0–3·0 for SARS-CoV and the 1918 influenza pandemic, 0·9 for MERS-CoV, and 1·5 for the 2009 influenza pandemic. In their viewpoint, the authors postulate that historical evidence from prior influenza pandemics indicates that pandemics tend to come in waves over the first 2–5 years as population immunity builds-up (naturally or through vaccination) and that this is the most likely trajectory for SARS-CoV-2. A combination of physical distancing, enhanced testing, quarantine, and contact tracing will be needed for a long time.
4 July
Yu X, Wei D, Chen Y, et al. Retrospective detection of SARS-CoV-2 in hospitalized patients with influenza-like illness. Emerging Microbes & Infections 2020, Full-text: https://doi.org/10.1080/22221751.2020.1785952
No cryptic transmission before early officially confirmed cases. In this retrospective screening for SARS-CoV-2 RNA in 1,271 nasopharyngeal swab samples, as well as the prevalence of IgM, IgG, and total antibodies against SARS-CoV-2 in 357 matched serum samples collected from hospitalized patients with influenza-like illness between December 1, 2018 and March 31, 2020 in Shanghai Ruijin Hospital, the onset date of the earliest COVID-19 case was January 25.
3 July
Cheng SY, Wang J, Shen AC, et al. How to Safely Reopen Colleges and Universities During COVID-19: Experiences From Taiwan. Ann Int Med 2020, Jul 2. Full-text: https://doi.org/10.7326/M20-2927
Reopening colleges and universities poses a special challenge worldwide. Taiwan is one of the few countries where schools are functioning normally. To secure the safety of students and staff, the Ministry of Education in Taiwan established general guidelines, including a combination of strategies such as – our future? – active campus-based screening and access control; school-based screening and quarantine protocols; student and faculty quarantine when warranted; mobilization of administrative and health center staff; regulation of dormitories and cafeterias; and reinforcement of personal hygiene, environmental sanitation, and indoor air ventilation practices. Somewhat depressing, but necessary?
Callaghan AW, Chard AN, Arnold P, et al. Screening for SARS-CoV-2 Infection Within a Psychiatric Hospital and Considerations for Limiting Transmission Within Residential Psychiatric Facilities – Wyoming, 2020. MMWR Morb Mortal Wkly Rep. 2020 Jul 3;69(26):825-829. PubMed: https://pubmed.gov/32614815. Full-text: https://doi.org/10.15585/mmwr.mm6926a4
Following admission of two patients with SARS-CoV-2 infection on April 13, 2020, in the absence of specific guidance on prevention and management of COVID-19 in psychiatric facilities, the state hospital implemented expanded admission screening and infection prevention and control procedures. The results of the point prevalence survey, indicating no further transmission among patients and HCW almost 3 weeks after admission of the two SARS-CoV-2-positive patients, suggested that the expanded procedures might have been effective.
1 July
Tenforde MW, Billig Rose E, Lindsell CJ, et al. Characteristics of Adult Outpatients and Inpatients with COVID-19 – 11 Academic Medical Centers, United States, March-May 2020. MMWR Morb Mortal Wkly Rep. 2020 Jul 3;69(26):841-846. PubMed: https://pubmed.gov/32614810. Full-text: https://doi.org/10.15585/mmwr.mm6926e3
Telephone interviews in a random sample of 350 adults aged ≥ 18 years who had positive RT-PCR in outpatient and inpatient settings at 11 U.S. academic medical centers in nine states revealed that only 46% were aware of recent close contact with someone with COVID-19, highlighting a need for increased screening, case investigation, contact tracing, and isolation of infected persons during periods of community transmission. Of note, approximately one third of symptomatic outpatients reported that they had not returned to baseline health by the interview date 14–21 days after testing positive.
30 June
Njuguna H, Wallace M, Simonson S, et al. Serial Laboratory Testing for SARS-CoV-2 Infection Among Incarcerated and Detained Persons in a Correctional and Detention Facility — Louisiana, April–May 2020. MMWR Morb Mortal Wkly Rep. ePub: 29 June 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6926e2
High COVID-19 attack rates can occur in correctional and detention facilities. During May 7–21, among 98 incarcerated and detained persons in Louisiana who were quarantined because of virus exposure, 71 (72%) had lab-confirmed SARS-CoV-2 infection identified through serial testing, among them 45% without any symptoms at the time of testing. These findings suggest ongoing transmission among quarantined persons living in close settings; therefore, serial testing of contacts of persons with COVID-19 in correctional and detention facilities can identify asymptomatic and presymptomatic persons who would be missed through symptom screening alone.
Brown NE, Bryant-Genevier J, Bandy U, Browning CA, Berns AL, Dott M, et al. Antibody responses after classroom exposure to teacher with coronavirus disease, March 2020. Emerg Infect Dis. 2020 Sep [date cited]. https://doi.org/10.3201/eid2609.201802
No big surprise: classroom interaction between an infected teacher and students might result in virus transmission. After returning from Europe to the United States on March 1, 2020, a symptomatic teacher received positive test results. In total 2/21 students exposed to the teacher in the classroom had positive serologic results.
Pulla P. ‘The epidemic is growing very rapidly’: Indian government adviser fears coronavirus crisis will worsen. Nature 2020, June 26. Full-text: https://www.nature.com/articles/d41586-020-01865-w
Interview with Jayaprakash Muliyil, an epidemiologist and advisor of the Indian government, providing insight into the epidemic in India where the virus seems to spread much faster and the infection rates are higher. A discussion on why officials in some badly affected cities seem reluctant to say that outbreaks are being driven by community transmission — where cases cannot be linked to known sources.
29 June
Nagler AR, Goldberg ER, Aguero-Rosenfeld ME, et al. Early Results from SARS-CoV-2 PCR testing of Healthcare Workers at an Academic Medical Center in New York City. Clin Inf Dis, June 28, 2020. Full-text: https://doi.org/10.1093/cid/ciaa867
Widespread testing of HCW offers valuable information for hospital workflow and workforce amid an epidemic that threatened to overwhelm the healthcare system. Over eight weeks, 14,764 employees were tested: 33% of employees were symptomatic, 8% of asymptomatic employees reported COVID-19 exposure, 3% of employees returning to work were antibody-positive. Positivity rates declined over time.
Hong LX, Lin A, He ZB, et al. Mask wearing in pre-symptomatic patients prevents SARS-CoV-2 transmission: An epidemiological analysis. Travel Med Infect Dis. 2020 Jun 24;36:101803. PubMed: https://pubmed.gov/32592903. Full-text: https://doi.org/10.1016/j.tmaid.2020.101803
The incidence of COVID-19 doubled (19.0% vs. 8.1%) for local residents who had close contact with people returning from Wuhan, who did not wear masks and turned out to be pre-symptomatic COVID-19 patients. In this study, a cluster of 21 local COVID-19 patients originated from a couple returning from Wuhan who played cards sequentially in a space-limited Chess and Card Room or who were living together over a longer-term with pre-symptomatic or asymptomatic relatives. No bridge for grandma during these days.
27 June
Horton R. Offline: The second wave. Lancet 2020, June 27, 395, ISSUE 10242, P1960. Full-text: https://doi.org/10.1016/S0140-6736(20)31451-3
Not in a good mood today? Then don’t read this important comment on what will likely happen during the next months. The first wave of the 1918 influenza pandemic took place between March and July. It proved relatively mild. The second wave arrived in August. It was much worse. Most of the 50–100 million deaths caused by influenza took place during 13 weeks between September and December, 1918. In many countries, the test, trace, and isolate system is still not fully functional and we have angry debates about whether physical distancing should be 1 m or 2 m. Scientists predict that a second wave will arrive in September, peaking by the end of 2020. Just sayin’.
25 June
Lewis M, Sanchez R, Auerbach S, et al. COVID-19 Outbreak Among College Students After a Spring Break Trip to Mexico — Austin, Texas, March 26–April 5, 2020. MMWR Morb Mortal Wkly Rep. ePub: 24 June 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6926e1
A college spring break trip mid-March led to 64 cases (14 asymptomatic and 50 symptomatic at the time of testing), including 60 among 183 vacation travelers, one among 13 household contacts, and three among 35 community contacts. Asymptomatic persons or those with mild symptoms likely played an important role in sustaining transmission. Prompt epidemiologic investigation contributed to outbreak control.
24 June
Britton T, Ball F, Trapman P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science 23 Jun 2020. Full-text: https://doi.org/10.1126/science.abc6810
43%, not 60%: Disease-induced herd immunity may be achieved at a substantially lower percentage than the classical herd immunity level derived from mathematical models assuming homogeneous immunization. The model indicates a reduction of herd immunity from 60% under homogeneous immunization down to 43% (assuming R0 = 2.5) in a structured population, but this should be interpreted as an illustration, rather than an exact value or even a best estimate.
22 June
Percivalle E, Cambiè G, Cassaniti I, et al. Prevalence of SARS-CoV-2 specific neutralising antibodies in blood donors from the Lodi Red Zone in Lombardy, Italy, as at 06 April 2020. Euro Surveill. 2020;25(24. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.24.2001031
This study evaluated SARS-CoV-2 RNA and neutralizing antibodies in blood donors (BD) residing in the highly affected “Lodi Red Zone”, Italy (an area of 169 km2, including 10 municipalities and 51,500 inhabitants, which went into lockdown in February 2020). Of 390 BDs recruited after 20 February − when the first COVID-19 case in Lombardy was identified, 91 (23%) aged 19–70 years were antibody positive.
Savulescu J, Cameron J. Why lockdown of the elderly is not ageist and why levelling down equality is wrong. J Med Ethics. 2020 Jun 19:medethics-2020-106336. PubMed: https://pubmed.gov/32561661. Full-text: https://doi.org/10.1136/medethics-2020-106336
Some intelligent thoughts on a “partial” lockdown for the elderly. The authors think that ethically, selective isolation is permissible. It is not unjust discrimination. It is analogous to only screening women for breast cancer: selecting those at a higher probability of suffering from a disease. Even if it were unjust discrimination, it would be proportionate because it brings benefits to the elderly and is necessary given the grave risks to the economy and subsequent well-being of the larger population of an indiscriminate lockdown. To oppose selective isolation of the elderly is to engage in a levelling down of equality which is itself morally questionable. There is no Hollywood happy ending here where everyone is a winner. Everything has its upsides and its downsides.
21 June
Twahirwa Rwema JO, Diouf D, Phaswana-Mafuya N, et al. COVID-19 Across Africa: Epidemiologic Heterogeneity and Necessity of Contextually Relevant Transmission Models and Intervention Strategies. Ann Intern Med. 2020 Jun 18. PubMed: https://pubmed.gov/32551812. Full-text: https://doi.org/10.7326/M20-2628
Brief overview on the burden and outcomes associated with COVID-19 in Africa, showing substantial variations across countries. Some explanations why many multiple mathematical models have failed to project the epidemic on the continent.
Han X, Wei X, Alwalid O, et al. Severe Acute Respiratory Syndrome Coronavirus 2 among Asymptomatic Workers Screened for Work Resumption, China. Emerg Infect Dis. 2020 Jun 17;26(9). PubMed: https://pubmed.gov/32553070. Full-text: https://doi.org/10.3201/eid2609.201848
It’s not completely gone. After the outbreak in Wuhan, China, the authors assessed 29,299 workers screened with PCR during March 13–April 25, 2020. They noted 18 (0.06%) cases of asymptomatic infection; 13 turned negative within 8.0 days, and 41 close contacts tested negative. Of 22,633 persons tested for SARS-CoV-2 antibodies, 617 (2.7%) cases had positive IgG but negative IgM; 196 (0.87%) cases had positive IgG and IgM; and 40 (0.18%) cases had negative IgG but positive IgM.
Czeisler MÉ, Tynan MA, Howard ME, et al. Public Attitudes, Behaviors, and Beliefs Related to COVID-19, Stay-at-Home Orders, Nonessential Business Closures, and Public Health Guidance – United States, New York City, and Los Angeles, May 5-12, 2020. MMWR Morb Mortal Wkly Rep. 2020 Jun 19;69(24):751-758. PubMed: https://pubmed.gov/32555138. Full-text: https://doi.org/10.15585/mmwr.mm6924e1
Most people agree: during the week of May 5–12, 2020, a survey among 2,402 adults in New York City and Los Angeles and broadly across the United States found widespread support of stay-at-home orders and nonessential business closures and high degree of adherence to COVID-19 mitigation guidelines. 74-82% reported they would not feel safe if these restrictions were lifted nationwide at the time the survey was conducted. In addition, among those who reported that they would not feel safe, some indicated that they would nonetheless want community mitigation strategies lifted and would accept associated risks (13-17%, respectively).
20 June
Truelove S, Abrahim O, Altare C, et al. The potential impact of COVID-19 in refugee camps in Bangladesh and beyond: A modeling study. PLoS Med 2020 Jun 16;17(6):e1003144. PubMed: https://pubmed.gov/32544156. Full-text: https://doi.org/10.1371/journal.pmed.1003144
Bangladesh hosts almost 1 million Rohingya refugees from Myanmar, with 600,000 concentrated in the Kutupalong-Balukhali Expansion Site. Using different transmission models and considering the age distribution in the camp, the authors expect 2,040-2,880 deaths (assuming that age was the primary determinant of infection severity and hospitalization). They also expect that comorbidities, limited hospitalization, and intensive care capacity may increase this risk.
19 June
Emeruwa UN, Ona S, Shaman JL, et al. Associations Between Built Environment, Neighborhood Socioeconomic Status, and SARS-CoV-2 Infection Among Pregnant Women in New York City. JAMA 2020, June 18, 2020. Full-text: https://doi.org/10.1001/jama.2020.11370
This cross-sectional study of 396 pregnant New York City residents delivering at New York hospitals showed that the likelihood of SARS-CoV-2 varied substantially across measures of built environment and neighborhood socioeconomic status. Large household membership, household crowding, and low socioeconomic status were associated with a 2-3 fold higher risk of infection.
Devi S. COVID-19 resurgence in Iran. Lancet 2020, June 20, 2020. Full-text: https://doi.org/10.1016/S0140-6736(20)31407-0
Brief overview. Iran was one of the first countries to experience a COVID-19 epidemic, and began relaxing restrictions in April. Cases dropped, with fewer than 1000 new cases per day by the start of May, but daily cases have since increased, with the Iranian Health Ministry reporting 2,410 new cases on June 13.
Clapham H, Hay J, Routledge I, et al. Seroepidemiologic Study Designs for Determining SARS-COV-2 Transmission and Immunity. Emerg Infect Dis. 2020 Jun 16;26(9). PubMed: https://pubmed.gov/32544053. Full-text: https://doi.org/10.3201/eid2609.201840
Numerous challenges exist in terms of sample collection, what the presence of antibodies actually means, and appropriate analysis and interpretation to account for test accuracy and sampling biases. The authors review strengths and limitations of different assay types and study designs, and discuss methods for rapid sharing and analysis of serologic data.
18 June
Soriano V, Meiriño R, Corral O, Guallar MP. SARS-CoV-2 antibodies in adults in Madrid, Spain. Clin Infect Dis. 2020 Jun 16:ciaa769. PubMed: https://pubmed.gov/32544951. Full-text: https://doi.org/10.1093/cid/ciaa769
Madrid has been the most deeply hit region by COVID-19 in Spain, with 65,000 confirmed cases and 9,000 deaths up to May 10th, eight weeks after the country’s lockdown had been implemented on March 14th. The authors found that roughly 10.9% of adults in Madrid (excluding those living in communities of 10 to 25 persons) had SARS-CoV-2 antibodies at the time of lockdown release on May 10th.
17 June
Davies NG, Klepac P, Liu Y et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med 2020, June 16. https://doi.org/10.1038/s41591-020-0962-9 l (Important)
Do children have a lower susceptibility to infection? Probably yes. The authors used epidemic data from Canada, China, Italy, Japan, Singapore, and South Korea to determine the level of susceptibility and clinical symptoms in various age groups. Susceptibility to infection in individuals under 20 years of age was approximately half that of adults aged over 20 years, and clinical symptoms manifest in 21% (95% confidence interval: 12–31%) of infections in 10- to-19-year-olds, rising to 69% (57–82%) of infections in people aged over 70 years. These estimates have implications for the expected global burden of COVID-19, as a result of demographic differences across settings.
Kucharski AJ, Klepac P, Conlan AJ, et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. The Lancet Infectious Diseases 2020 Published: June 16, 2020. Full-text: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30457-6/fulltext
Another mathematical modelling study, using pandemic data from 40,162 UK participants and simulating the effect of a range of different testing, isolation, tracing, and physical distancing scenarios. If combined with moderate physical distancing measures, self-isolation and contact tracing would be more likely to achieve control of SARS-CoV- 2 transmission.
16 June
Stoke EK, Zambrano LD, Anderson KN. Coronavirus Disease 2019 Case Surveillance — United States, January 22–May 30, 2020. MMWR June 15, 2020. Full-text: https://www.cdc.gov/mmwr/volumes/69/wr/mm6924e2.htm
A detailed picture of the epidemic in the US. This report describes demographic characteristics, underlying health conditions, symptoms, and outcomes among 1,320,488 laboratory-confirmed COVID-19 cases individually reported to CDC during January 22–May 30, 2020. Some key messages: Overall, 14% of patients were hospitalized, 2% were admitted to an intensive care unit (ICU), and 5% died. Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were non-Hispanic American Indian or Alaska Native. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic.
Thornton J. Covid-19: Africa’s case numbers are rising rapidly, WHO warns. BMJ 2020; 369. Full-text: https://doi.org/10.1136/bmj.m2394
A brief but concerning review on the situation in Africa. Since the virus was first detected in Egypt on 14 February, it took 98 days to reach 100,000 cases and only 18 days to move to 200,000 cases on the continent. More than 5,600 people have died from the illness, 70% of whom were in just five countries: Algeria, Egypt, Nigeria, South Africa, and Sudan.
15 June
Mubarak N, Zin CS. Religious tourism and mass religious gatherings – The potential link in the spread of COVID-19. Current perspective and future implications. Travel Med Infect Dis. 2020 Jun 9;36:101786. PubMed: https://pubmed.gov/32531422. Full-text: https://doi.org/10.1016/j.tmaid.2020.101786
Important comment on mass religious gatherings. The authors recommend restrictions on the entry of Hajj pilgrims who are from epicentres and hotspots, from countries with suboptimal disease surveillance systems or with inadequate quarantine and diagnostic infrastructure for returning pilgrims who are over 50 years old or suffer from chronic disease, ie patients with diabetes and cardiovascular complications. Saudi Arabia needs to deploy a pre-emptive approach. We’ll see whether this is feasible.
Habib H. Has Sweden’s controversial covid-19 strategy been successful? BMJ 2020; 369. Full-text: https://doi.org/10.1136/bmj.m2376
Probably not. Some thoughts on Sweden’s controversial decision not to lock down the country. They are still far away from herd immunity (an ongoing nationwide study on 20 May found that just 7.3% of Stockholm residents had developed antibodies) and the death toll is immense.
Okell LC, Verity R, Watson OJ, et al. Have deaths from COVID-19 in Europe plateaued due to herd immunity? Lancet. 2020 Jun 11:S0140-6736(20)31357-X. PubMed: https://pubmed.gov/32534627. Full-text: https://doi.org/10.1016/S0140-6736(20)31357-X
No. Epidemiological data suggest that no country has yet seen infection rates sufficient to prevent a second wave of transmission, should controls or behavioural precautions be relaxed without compensatory measures in place.
13 June
Walker PG, Whittaker C, Watson OJ, et al. The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science 12 Jun 2020. Full-text: https://DOI.ORG/10.1126/science.abc0035
An in-depth analysis of the potential impact of the pandemic in low- and middle-income countries (LMIC). The analysis gives insight into how differences in demography, social structure and health care availability and quality combine and potentially influence the impact of measures that can help reduce the spread of the virus. However, the bottom line is: We don’t know yet. On one hand, we have an overall younger population and a shorter time for lockdown measures to be in place in LMIC. On the other hand, there is a higher burden of infectious diseases such as AIDS and TB already, and of poverty-related determinants of poorer health outcomes such as malnutrition. There is also a more persistent spread to older age categories (higher levels of household-based transmissions) and poorer quality health care and lack of health care capacity.
Oreshkova N, Molenar RJ, Vremen S. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Eurosurveillance 2020, June 11. Volume 25, Issue 23. Full-text: https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.23.2001005
Despite a law approved by the Dutch parliament in 2012 that will ban mink farming as of 2024 for ethical reasons, there are still around 125 mink farms in the Netherlands, with an average of 5,000 female breeding animals. In 2019, 4 million minks were “produced”. This article describes several outbreaks on these farms. Detection of viral RNA in the airborne inhalable dust clearly suggests dust and/or droplets as means of transmission between the minks and occupational risk of exposure for the workers on the farms. On 3 June, the Dutch Ministry of Agriculture decided to cull all minks of SARS-CoV-2-infected farms, starting on 5 June. This may be the right time to speed up the final ban.
12 June
Furuse Y, Sando E, Tsuchiya N, et al. Clusters of Coronavirus Disease in Communities, Japan. January-April 2020. Emerg Infect Dis. 2020 Jun 10;26(9). PubMed: https://pubmed.gov/32521222. Full-text: https://doi.org/10.3201/eid2609.202272
Bye, bye, karaoke. The Japanese authors defined a cluster as > 5 cases with primary exposure reported at a common event or venue, excluding within-household transmissions. In total, 61 COVID-19 clusters were found in various communities in the country: 18 (30%) in healthcare facilities; 10 (16%) in care facilities of other types, such as nursing homes and day care centers; 10 (16%) in restaurants or bars; 8 (13%) in workplaces; 7 (11%) in music-related events, such as live music concerts, chorus group rehearsals, and karaoke parties; 5 (8%) in gymnasiums; 2 (3%) in ceremonial functions; and 1 (2%) in transportation-related incident in an airplane. Of note, 41% of probable primary case-patients were pre-symptomatic or asymptomatic at the time of transmission. 45% had cough. Many clusters were associated with heavy breathing in close proximity.
Stringhini S, Wisniak A, Piumatti G, et al. The Lancet, June 11, 2020. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Full-text: https://doi.org/10.1016/S0140-6736(20)31304-0
Geneva was a COVID-19 hot spot in Switzerland (5000 cases over < 2,5 months in half a million people). Authors performed 5 consecutive weekly sero-surveys among 2,766 randomly selected participants from a previous population-representative survey, and 1,339 household members aged 5 years and older. Each participant was tested for anti-SARS-CoV-2-IgG antibodies. Seroprevalence increased from about 5% to about 11%. Of note, young children (5–9 years) and older people (≥ 65 years) had significantly lower seroprevalence than the other age groups. Authors estimated that there were 11 infections for every COVID-19 confirmed case.
11 June
ECDC Public Health Emergency Team, Danis K, Fonteneau L, et al. High impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA. May 2020. Eurosurveillance, Volume 25, Issue 22, 04/Jun/2020 Article. Full-text: https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.22.2000956
Residents in long-term care facilities contribute 30–60% of all COVID-19 deaths in many European countries. This article provides an overview of the importance of surveillance and infection prevention and control measures, in order to identify clusters early, decrease the spread within and between facilities and reduce the size and severity of outbreaks.
Enserink M. Coronavirus rips through Dutch mink farms, triggering culls to prevent human infections. Science Mag 2020, June 9. Full-text: https://www.sciencemag.org/news/2020/06/coronavirus-rips-through-dutch-mink-farms-triggering-culls-prevent-human-infections
Sad story on several outbreaks at Dutch mink farms. That mink are susceptible wasn’t a surprise, because they are closely related to ferrets. Once COVID-19 reaches a farm, the virus appears to spread like wildfire, even though the animals are housed in separate cages. The government decided to cull thousands of animals because the problem could become bigger in the months ahead.
10 June
Payne DC, Smith-Jeffcoat SE, Nowak G, et al. SARS-CoV-2 Infections and Serologic Responses from a Sample of U.S. Navy Service Members — USS Theodore Roosevelt, April 2020. MMWR Morb Mortal Wkly Rep. ePub: 9 June 2020. Full-text: https://www.cdc.gov/mmwr/volumes/69/wr/mm6923e4.htm
In late March 2020, a large outbreak on the aircraft carrier USS Theodore Roosevelt was characterized by widespread transmission with relatively mild symptoms and asymptomatic infection among mostly young, healthy adults with close, congregate exposures. One fifth of infected participants reported no symptoms. Preventive measures, such as using face-coverings and observing social distancing, reduced risk for infection: among 382 service members, those who reported taking preventive measures had a lower infection rate than did those who did not report taking these measures (e.g., wearing a face-covering, 56% versus 81%; avoiding common areas, 54% versus 68%; and observing social distancing, 55% versus 70%, respectively).
9 June
Flaxman S, Mishra S, Gandy A, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020 Jun 8. PubMed: https://pubmed.gov/32512579. Full-text: https://doi.org/10.1038/s41586-020-2405-7 l (Important)
This world-leading group of epidemiologists and statisticians estimated the total infection rates across 11 European countries. Main results: between 12 and 15 million individuals have been infected with SARS-CoV-2 up to May 4th, representing between 3.2% and 4.0% of the population. Percentages of total population infected were for Austria 0.76% (0.59% – 0.98%), Belgium 8.0 % (6.1% – 11%), Denmark 1.0% (0.81% – 1.4%), France 3.4% (2.7% – 4.3%), Germany 0.85% (0.66% – 1.1%), Italy 4.6% (3.6% – 5.8%), Norway 0.46% (0.34% – 0.61%), Spain 5.5% (4.4% – 7.0%), Sweden 3.7% (2.8% – 5.1%), Switzerland 1.9% (1.5% – 2.4%) and United Kingdom 5.1% (4.0% – 6.5%). Results also showed that major non-pharmaceutical interventions and lockdown in particular have had a large effect on reducing transmission.
Deng X, Gu W,Federman S, et al. Genomic surveillance reveals multiple introductions of SARS-CoV-2 into Northern California. Science 08 Jun 2020. Full-text: https://doi.org/10.1126/science.abb9263
Detective work, analysing the genomic epidemiology of SARS-CoV-2 in Northern California from late January to mid-March 2020, using samples from 36 patients spanning 9 counties and the Grand Princess cruise ship. Phylogenetic analyses revealed the cryptic introduction of at least 7 different SARS-CoV-2 lineages into California, including epidemic WA1 strains associated with Washington State, with a lack of predominant lineage, and limited transmission between communities.
8 June
Xu X, Sun J, Nie S, et al. Seroprevalence of immunoglobulin M and G antibodies against SARS-CoV-2 in China. Nat Med. 2020 Jun 5. PubMed: https://pubmed.gov/32504052. Full-text: https://doi.org/10.1038/s41591-020-0949-6
To estimate the cumulative prevalence, authors evaluated IgM and IgG antibodies in 17,368 individuals from Wuhan, China. The seropositivity in Wuhan was low, varying between 3.2% and 3.8% in different sub-cohorts. As seen in other studies, an early and a higher level of IgG response was observed, compared to IgM.
Graham N, Junghans C, Downes R, et al. SARS-CoV-2 infection, clinical features and outcome of COVID-19 in United Kingdom nursing homes. J Infect. 2020 Jun 3:S0163-4453(20)30348-0. PubMed: https://pubmed.gov/32504743. Full-text: https://doi.org/10.1016/j.jinf.2020.05.073
Outbreak investigation involving 394 residents and 70 staff in 4 nursing homes in central London. Overall, 26% of residents died over a two-month period. Systematic testing identified 40% of residents as positive for SARS-CoV-2 and of these, 43% were asymptomatic and 18% had only atypical symptoms during the two weeks prior to testing. Of note, this was also true of many residents in the days leading up to death indicating that even in severe COVID-19, fever and cough were commonly absent. 4% of asymptomatic staff also tested positive.
7 June
Li Z, Chen Q, Feng L, et al. Active case finding with case management: the key to tackling the COVID-19 pandemic. The Lancet, June 4, 2020. https://doi.org/10.1016/S0140-6736(20)31278-2
Learning from China. Case finding and management, with identification and quarantine of close contacts: the authors describe the next steps planned in China following the containment effort.
4 June
Davies NG, Kucharski ADJ, Eggo RM, et al. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet, June 02, 2020. Full-text: https://doi.org/10.1016/S2468-2667(20)30133-X
Herd immunity? Forget it. Using a stochastic age-structured transmission model to explore a range of intervention scenarios, tracking 66 million people in England, Wales, Scotland, and Northern Ireland, the authors projected a median unmitigated burden of 23 million (95% prediction interval 13–30) clinical cases and 350,000 deaths (170,000–480, 000) due to COVID-19 in the UK by December, 2021. Bad news because extreme measures are probably required to bring the epidemic under control.
2 June
Lee H, Lee H, Song KH, et al. Impact of Public Health Interventions on Seasonal Influenza Activity During the SARS-CoV-2 Outbreak in Korea. Clin Infect Dis. 2020. PubMed: https://pubmed.gov/32472687. Full-text: https://doi.org/10.1093/cid/ciaa672
Efforts to activate high level national response not only led to a decrease in COVID-19, but also a substantial decrease in seasonal influenza activity. During the period of enforced social distancing from week 9 to 17 of 2020 in Korea, influenza hospitalization cases were 11.9-26.9-fold lower compared with previous seasons. This is good news, because nobody needs influenza.
Transmission
Ragan I, Hartson L, Pidcoke H, Bowen R, Goodrich R. Pathogen reduction of SARS-CoV-2 virus in plasma and whole blood using riboflavin and UV light. PLoS One. 2020 May 29;15(5. PubMed: https://pubmed.gov/32470046. Full-text: https://doi.org/10.1371/journal.pone.0233947. eCollection 2020
Plasma and whole blood units infected with SARS-CoV-2 underwent treatment with riboflavin and UV light. Riboflavin and UV light effectively reduced the titer of SARS-CoV-2 to the limit of detection in human plasma and by 3.30 ± 0.26 on average in whole blood. This is good news, because these treatments may reduce blood-borne pathogens in high-risk settings while maintaining blood product quality.
Nagano T, Arii J, Nishimura M, et al. Diligent medical activities of a publicly designated medical institution for infectious diseases pave the way for overcoming COVID-19: A positive message to people working at the cutting edge. Clin Infect Dis. 2020 May 31. PubMed: https://pubmed.gov/32474577. Full-text: https://doi.org/10.1093/cid/ciaa694
Of 509 medical staff members working to treat COVID-19 patients at the Hyogo Prefectural Kakogawa Medical Center, a large medical institution for infectious diseases in Japan (mean number of hospitalized COVID-19 patients was 20), none had IgG antibodies for SARS-CoV-2 on May 1-8. This is good news, because results show that standard preventive measures against infectious diseases can prevent SARS-CoV-2 exposure in medical staff.
1 June
Dora AV, Winnett A, Jatt LP, et al. Universal and Serial Laboratory Testing for SARS-CoV-2 at a Long-Term Care Skilled Nursing Facility for Veterans – Los Angeles, California, 2020. MMWR Morb Mortal Wkly Rep. 2020 May 29;69(21):651-655. PubMed: https://pubmed.gov/32463809. Full-text: https://doi.org/10.15585/mmwr.mm6921e1
Again and again: Test them all, immediately. On March 28, 2020, two residents of a long-term care skilled nursing facility in Los Angeles had positive test results. From March 29-April 23, all residents, regardless of symptoms, underwent serial (approximately weekly) nasopharyngeal PCR testing. 19/99 (19%) residents and 8/136 (6%) staff members had positive test results. 14/19 residents were asymptomatic at the time of testing. Among these, eight developed symptoms 1-5 days after specimen collection and were later classified as presymptomatic.
Looi MK. Covid-19: Japan ends state of emergency but warns of “new normal”. BMJ. 2020 May 26;369:m2100. PubMed: https://pubmed.gov/32457055. Full-text: https://doi.org/10.1136/bmj.m2100
Japan has done a good job. This article explains why. Public adherence to the rules, along with cluster tracing and a ban on mass gatherings, seems to have achieved success in bringing the outbreak under control, alongside widespread mask use and hygiene being a normal part of Japanese etiquette. Japan has ended its state of emergency a week after its new infections fell below 50 a day.
31 May
Jorden MA, Rudman SL, et al. Evidence for Limited Early Spread of COVID-19 Within the United States, January–February 2020. MMWR Morb Mortal Wkly Rep. 29 May 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6922e1
Information from diverse data sources suggests that limited community transmission of SARS-CoV-2 in the United States occurred between the latter half of January and the beginning of February, following an importation from China. This importation initiated a lineage, the Washington State clade, which subsequently spread throughout the Seattle metropolitan area and possibly elsewhere. Several importations of SARS-CoV-2 from Europe followed in February and March. Of note, overall disease incidence before February 28 was too low to be detected through emergency department syndromic surveillance data.
Sehra ST, Salciccioli JD, Wiebe DJ, Fundin S, Baker JF. Maximum Daily Temperature, Precipitation, Ultra-Violet Light and Rates of Transmission of SARS-Cov-2 in the United States. Clin Infect Dis. 2020 May 30. PubMed: https://pubmed.gov/32472936. Full-text: https://doi.org/10.1093/cid/ciaa681
Transmission is likely to remain high at warmer temperatures. Using negative binomial regression modelling, authors investigated whether daily maximum temperature, precipitation and UV index were related to COVID-19 incidence. Incidence declined with increasing temperature up to 52°F and was somewhat lower at warmer versus cooler temperatures. However, the association between temperature and transmission was small.
30 May
Gonzalez-Reiche AS, Hernandez MM, Sullivan MJ, et al. Introductions and early spread of SARS-CoV-2 in the New York City area. Science 29 May 2020: eabc1917. Full-text: https://doi.org/10.1126/science.abc1917
A first analysis of the SARS-CoV-2 viral genotypes collected from patients seeking medical care in the New York City metropolitan area. Main message: The NYC epidemic has been mainly sourced from untracked transmission between the US and Europe, with limited evidence of direct introductions from China where the virus originated. Isolates were distributed throughout the phylogenetic tree; consistent with multiple independent introductions.
Sen S, Karaca-Mandic P, Georgiou A. Association of Stay-at-Home Orders With COVID-19 Hospitalizations in 4 States. JAMA May 27, 2020. Full-text: https://10.1001/jama.2020.9176
Staying at home works. In 4 US states (Colorado, Minnesota, Ohio, and Virginia) with stay-at-home orders, cumulative hospitalizations for COVID-19 deviated from projected best-fit exponential growth rates after these orders became effective. The deviation started 2 to 4 days sooner than the median effective date of each state’s order and may reflect the use of a median incubation period for symptom onset and time to hospitalization to establish this date.
29 May
Ball P, Maxmen A. The epic battle against coronavirus misinformation and conspiracy theories. Nature 2020, 581, 371-374. Full-text: https://doi.org/10.1038/d41586-020-01452-z
This article shows how analysts and researchers have been scrambling to track and analyse the disparate falsehoods floating around — both ‘misinformation’, which is wrong but not deliberately misleading, and ‘disinformation’, which refers to organized falsehoods that are intended to deceive. Inaccurate information doesn’t only mislead, but could be a matter of life and death if people start taking unproven drugs, ignoring public-health advice, or refusing a coronavirus vaccine if one becomes available.
Lam TT. Tracking the genomic footprints of SARS-CoV-2 transmission. Trends in Genetics 2020. Full-text: https://doi.org/10.1016/j.tig.2020.05.009
Analysis of SARS-CoV-2 genomes provides insights into the origin, transmission, spread and evolution. Brief review on current knowledge and research.
28 May
Larochelle MR. “Is It Safe for Me to Go to Work?” Risk Stratification for Workers during the Covid-19 Pandemic. N Engl J Med. 2020 May 26. PubMed: https://pubmed.gov/32453518. Full-text: https://doi.org/10.1056/NEJMp2013413
A simple framework to help clinicians counsel patients about continuing to work in the midst of the pandemic based on their occupational risk of contracting SARS-CoV-2 and their risk of death if they are infected.
Campbell KH, Tornatore JM, Lawrence KE, et al. Prevalence of SARS-CoV-2 Among Patients Admitted for Childbirth in Southern Connecticut. JAMA. 2020 May 26. PubMed: https://pubmed.gov/32453390. Full-text: https://doi.org/10.1001/jama.2020.8904
From April 2, 2020, to April 29, 2020, screening and testing of patients admitted for childbirth was initiated at 3 Yale New Haven Health hospitals in southern Connecticut. Of 770 patients, 30 (3.9%) tested positive for SARS-CoV-2, of whom 22 (73%) were asymptomatic.
27 May
Randolph HE, Barreiro LB. Herd Immunity: Understanding COVID-19. Immunity Volume 52, ISSUE 5, P737-741, 2020. Full-text: https://doi.org/10.1016/j.immuni.2020.04.012
Overview on the basic concepts of herd immunity and its implications. There is no straightforward, ethical path to reach herd immunity, as the societal consequences of achieving it are devastating. Instead, an emphasis should be placed on policies that protect the most vulnerable groups in the hopes that herd immunity will eventually be achieved as a “byproduct” of such measures, although not the primary objective itself.
Honigsbaum M. Revisiting the 1957 and 1968 influenza pandemics. Lancet May 25, 2020. Full-text: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31201-0/fulltext
Were people really more stoic in 1918, 1957, and 1968? Or were there other factors that might account for the dampened social and emotional responses to these pandemics? And what should historians make of functionalist and, arguably, selective readings of history that seek to draw moral lessons from the past? This intelligent article has some interesting thoughts on these issues.
26 May
Peak CM, Kahn R, Grad YH, et al. Individual quarantine versus active monitoring of contacts for the mitigation of COVID-19: a modelling study. Lancet Infect Dis. 2020 May 20. PubMed: https://pubmed.gov/32445710. Full-text: https://doi.org/10.1016/S1473-3099(20)30361-3
Complex models, comparing individual quarantine (separation from others of an individual who is believed to be exposed to the disease but not currently showing symptoms) with active monitoring targeted by contact tracing (assessing for symptoms at regular intervals such as twice-daily visits by HCW or phone-based self-monitoring, and if symptoms are detected, the individual is promptly isolated). Bottom line: It depends. It depends on the assumptions regarding the serial interval, the amount of transmission that occurs before symptom onset, and the feasibility setting. With a short mean serial interval of 4.8 days and hence substantial pre-symptomatic infectiousness, individual quarantine was considerably more effective than active monitoring at reducing onward transmission. With longer serial intervals both active monitoring and individual quarantine effectively reduce transmission.
Liotta G, Marazzi MC, Orlando S. Is social connectedness a risk factor for the spreading of COVID-19 among older adults? The Italian paradox. PLOS May 21, 2020. Full-text:
One hypothesis about the fatal spread of SARS-CoV-2 in Italy is that the supposed closeness between younger and older generations in Italian families may have played a major role. In this study, this was not confirmed. Paradoxically, it seemed that the variables associated with social isolation were risk factors for higher rates among the elderly. Social relationships may be protective against increased mortality rates during a crisis impacting the frailest populations. Instead, availability of beds in nursing homes were one of the determinants of infection rate among individuals aged >80.
24 May
Le Quéré C, Jackson RB, Jones MW et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat Clim Chang 2020. Full-text: https://doi.org/10.1038/s41558-020-0797-x
The global CO2 emissions have decreased by 17% by early April 2020 compared with the mean 2019 levels, just under half from changes in surface transport (cars, truck, buses). More than one billion tons of carbon emissions less. At their peak, emissions in individual countries decreased by an average of 26%, admittedly extreme and probably unseen before, but just to the level of emissions in 2006. The impact on 2020 annual emissions will depend on the duration of the confinement, with a low estimate of –4% if pre-pandemic conditions return by mid-June, and a high estimate of –7% if some restrictions remain worldwide until the end of 2020. These figures are comparable to the rates of decrease needed year-on-year over the next decades to limit climate change to a 1.5 °C warming.
Memish ZA, Aljerian N, Ebrahim SH. Tale of three seeding patterns of SARS-CoV-2 in Saudi Arabia. Lancet Infect Dis. 2020 May 19:S1473-3099(20)30425-4. PubMed: https://pubmed.gov/32442522. Full-text: https://doi.org/10.1016/S1473-3099(20)30425-4
With regard to case numbers, Saudi Arabia already ranks #15 in the world. Beside routine travel, authors describe two factors driving the epidemic. First, each month about 1 million incoming pilgrims from 180 countries merge with about 1 million Saudi national Sunni pilgrims at Saudi Arabia’s two holy sites. Second is the returning Shiite Saudi national pilgrims (4·9 million Shiite population in Saudi Arabia) who travel to Iran for pilgrimage. Of note, men and woman older than 60 years are overrepresented among pilgrims. Bad prospects.
23 May
Kofler N, Baylis F. Ten reasons why immunity passports are a bad idea. Nature 2020, 581, 379-381. Full-text: https://doi.org/10.1038/d41586-020-01451-0
Forget the COVID pass! During the past weeks, we have shared several reasons why immunity passports are a bad idea. This commentary provides 10 more reasons. Restricting liberty on the basis of biology threatens freedom, fairness and public health.
Haushofer J, Metcalf JE. Which interventions work best in a pandemic? Science 21 May 2020: eabb6144. Full-text: https://doi.org/10.1126/science.abb6144
Randomized controlled trials can be used for non-pharmaceutical interventions. Surprisingly they have received little attention in the current pandemic, despite a long history in epidemiology and social science. In this interesting commentary, authors describe how RCTs can be practically and ethically implemented in a pandemic, how compartmental models from infectious disease epidemiology can be used to minimize measurement requirements, and how to control for spillover effects and harness their benefits.
22 May
Lyu W, Wehby GL. Comparison of Estimated Rates of Coronavirus Disease 2019 (COVID-19) in Border Counties in Iowa Without a Stay-at-Home Order and Border Counties in Illinois With a Stay-at-Home Order. JAMA Netw Open. 2020 May 1;3(5):e2011102. PubMed: https://pubmed.gov/32413112. Full-text: https://doi.org/10.1001/jamanetworkopen.2020.11102 l (Important)
Is it necessary to stay home during the epidemic’s peak? Probably, yes. This well-conducted study focused on the effects of a general stay-at-home-order. On March 21, Illinois did so while Iowa didn’t. Authors compared daily incidence in 8 Iowa counties bordering Illinois with those in the 7 Illinois counties bordering Iowa. Within a month after the stay-at-home order, the curves started to diverge considerably. Cases increased more quickly in Iowa and more slowly in Illinois, leading to an excess of about 30 % in Iowa counties. Sensitivity analyses addressing differences in timing of closing schools and nonessential businesses and differences in population density and poverty rates between the two states supported these findings.
Sood N, Simon P, Ebner P, et al. Seroprevalence of SARS-CoV-2–Specific Antibodies Among Adults in Los Angeles County, California, on April 10-11, 2020. JAMA. Published online May 18, 2020. Full-text: https://doi.org/10.1001/jama.2020.8279
No herd immunity in LA. Participants were offered testing at 6 study sites or at home in mid-April. Among 865 cases, the prevalence of antibodies was 4.65%. However, even this low number may be biased due to nonresponse or due to the fact that symptomatic persons may have been more likely to participate.
17 May
Banerjee A, Pasea L, Harris S, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020 May 12. PubMed: https://pubmed.gov/32405103. Full-text: https://doi.org/10.1016/S0140-6736(20)30854-0 – OurRisk.CoV (online tool): http://covid19-phenomics.org/PrototypeOurRiskCoV.html
The authors provide a simple model and an online tool for understanding excess mortality over 1 year from the COVID-19 pandemic, based on age, sex, and underlying condition-specific estimates. For the UK, 293,991 deaths would be expected in a “do-nothing scenario”. With mitigation (ie, less rigorous and voluntary measures), authors predict between 18,000 and 37,000 deaths.
16 May
Dehning K, Zierenberg , Spitzner FP. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science 15 May 2020. Full-text: https://doi.org/10.1126/science.abb9789
Focusing on the COVID-19 spread in Germany, these elegant models detected three change points in the effective growth rate that correlated well with interventions. First, the spreading rate decreased from 0.43 to 0.25, the decrease initiating around March 7 (cancellation of large public events, such as trade fairs and soccer matches). Second, the rate decreased further to 0.15 (around March 16, closure of schools, childcare facilities, non-essential stores). Third, the spreading rate decreased further to 0.09 (initiated around March 24, strict contact ban). While the first two change points were not sufficient to trigger a shift from the growth of novel cases to a decline, the third brought this crucial reversal. This model can be used for future scenarios – the code is freely available and can be readily adapted to any country. The paper also highlights the impact of time: delaying restrictions by only 5 days may have an incredible impact on case numbers. Sleep well, Boris, Jair, Mark etc.
14 May
Salje J, Kiem CT, Lefrancq N, et al. Estimating the burden of SARS-CoV-2 in France. Science 13 May 2020. Full-text: https://doi.org/10.1126/science.abc3517
A suite of modeling analyses was used to characterize the dynamics of SARS-CoV-2 transmission in France and the impact of the lockdown on these dynamics. The authors estimated that 3.6% of infected individuals were hospitalized and 0.7% died. The lockdown reduced the reproductive number from 2.90 to 0.67. By 11 May 2020, authors project 2.8 million infections in France (or 4.4% of the population (range: 2.8–7.2)). Population immunity appeared to be insufficient to avoid a second wave.
11 May
Tian H, Liu Y, Li Y, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020 May 8;368(6491):638-642. PubMed: https://pubmed.gov/32234804. Full-text: https://doi.org/10.1126/science.abb6105
Quantitative analysis of the impact of control measures between 31 December 2019 and 19 February 2020. Travel restrictions in and out of Wuhan were too late to prevent the spread of the virus. However, measures such as closing citywide public transport and entertainment venues and banning public gatherings combined to avert hundreds of thousands of cases of infection.
10 May
Weitz JS, Beckett SJ, Coenen AR, et al. Modeling shield immunity to reduce COVID-19 epidemic spread. Nat Med. 2020 May 7. PubMed: https://pubmed.gov/32382154. Full-text: https://doi.org/10.1038/s41591-020-0895-3
The authors propose an approach to limit transmission, which is both complementary to and intended to lessen the multifaceted costs of mitigation and suppression. The core idea is to leverage a mechanism of ‘interaction substitution’ by identifying recovered individuals who have protective antibodies and deploying them back into the community. The intention is to develop population-level ‘shield immunity’ by amplifying the proportion of interactions with recovered individuals relative to those of individuals of unknown status.
8 May
Wallace M, Hagan L, Curran KG, et al. COVID-19 in Correctional and Detention Facilities — United States, February–April 2020. MMWR Early Release, May 6, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6919e1.htm
First documentation of the epidemic in correctional and detention facilities. Aggregated data on COVID-19 cases reported to CDC by 37 of 54 state and territorial health department jurisdictions in the US. Prison bars do not work: As of April 21, 2020, 4,893 cases and 88 deaths among incarcerated and detained persons and 2,778 cases and 15 deaths among staff members have been reported.
Wells CR, Stearns JK, Lutumba P, Galvani AP. COVID-19 on the African continent. Lancet Infect Dis May 06, 2020. Full-text: https://doi.org/10.1016/S1473-3099(20)30374-1
Brief review. The transmissibility of SARS-CoV-2, combined with the scarcity of crucial health equipment and the challenges of implementing widespread physical distancing and case isolation, poses a grave threat to the African continent.
Fusaroli P, Balena S, Lisotti A. On the death of 100+ Italian doctors from COVID-19. Infection 2020. https://doi.org/10.1007/s15010-020-01436-1. Full-text: https://link.springer.com/article/10.1007/s15010-020-01436-1.
Authors speculate on the reasons why 95/100 of deceased Italian doctors were men. Could different habits between men and women have played a role too? According to some research, women are supposedly more scrupulous in performing hand hygiene than men.
7 May
Persad G, Emanuel EJ. The Ethics of COVID-19 Immunity-Based Licenses (“Immunity Passports”). JAMA. Published online May 6, 2020. Full-text: https://jamanetwork.com/journals/jama/fullarticle/2765836
Chile, Germany and the UK, among others, have indicated they will implement certifications that a person has contracted and recovered from COVID-19. According to the authors, immunity-based licenses require careful implementation to be ethical in practice. These “licenses” may allow immune people to engage in economic activity and safer care for vulnerable populations. However, major concerns remain as community licensing could stigmatize people, undermining the value of equal treatment. Businesses may use unregulated evidence of immunity, such as test results, or use assumptions about immunity or vulnerability that are likely to be arbitrary and biased.
Virology
Watanabe Y, Allen JD, Wrapp D, McLellan JS, Crispin M. Site-specific glycan analysis of the SARS-CoV-2 spike. Science. 2020 May 4. PubMed: https://pubmed.gov/32366695. Full-text: https://doi.org/10.1126/science.abb9983
The surface of the envelope spike is dominated by host-derived glycans. These glycans facilitate immune evasion by shielding specific epitopes from antibody neutralization. The SARS-CoV-2 S gene encodes 22 N-linked glycan sequons per protomer. Using a site-specific mass spectrometric approach, authors reveal these glycan structures on a recombinant SARS-CoV-2 S immunogen.
6 May
Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers: A Living Rapid Review. Ann Intern Med. 2020 May 5. PubMed: https://pubmed.gov/32369541. Full-text: https://doi.org/10.7326/M20-1632
This review summarizes the risk factors for coronavirus infections in HCWs. There was evidence that more consistent and full use of recommended PPE measures was associated with decreased risk for infection, suggesting a dose–response relationship. This association was most consistent for masks but was also observed for gloves, gowns, and eye protection, as well as handwashing. Some evidence was found that N95 masks might be associated with decreased risk for infection versus surgical masks. Evidence also indicated an association between certain exposures (such as involvement in intubations, direct contact with infected patients, or contact with bodily secretions).
Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020 May 4. PubMed: https://pubmed.gov/32365354. Full-text: https://doi.org/10.1038/s41586-020-2293-x
Another study on the impact of non-pharmaceutical interventions (NPIs) in China. Without NPIs, the COVID-19 cases would likely have shown a 67-fold increase (interquartile range 44-94) by February 29. Early detection and isolation of cases was estimated to have prevented more infections than travel restrictions and contact reductions, but combined NPIs achieved the strongest and most rapid effect. The lifting of travel restrictions does not appear to lead to an increase in cases if social distancing interventions are maintained.
3 May
Zhang J, Litvinova M, Liang Y, et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 29 Apr 2020: Full-text: https://science.sciencemag.org/content/early/2020/04/28/science.abb8001
An elegant model demonstrating the impact of lockdown by using contact survey data for Wuhan and Shanghai before and during the outbreak. Daily contacts were reduced 7-8-fold during the social distancing period, with most interactions restricted to the household. Of note, children 0-14 years were less susceptible to infection than adults (however, numbers were low). Social distancing alone, as implemented during the outbreak, was sufficient to control COVID-19. While proactive school closures cannot interrupt transmission on their own, they can reduce peak incidence by 40-60% and delay the epidemic.
Lu J, du Plessis L, Liu Z. Genomic Epidemiology of SARS-CoV-2 in Guangdong Province, China. Cell April 30, 2020. Full-text: https://www.cell.com/cell/fulltext/S0092-8674(20)30486-4
A comprehensive study on genomic epidemiology of SARS-CoV-2 in Guangdong province. The authors generated 53 genomes from infected individuals in Guangdong and deduce that following the first COVID-19 case detected in early January, most infections were the result of virus importation from elsewhere, and that chains of local transmission were limited in size and duration.
1 May
Jia JS, Lu X, Yuan Y. et al. Population flow drives spatio-temporal distribution of COVID-19 in China. Nature 2020. https://doi.org/10.1038/s41586-020-2284-y. Full-text: https://www.nature.com/articles/s41586-020-2284-y#citeas
When people move, they take contagious diseases with them. Using detailed mobile phone geolocation data to compute aggregate population movements, the authors tracked the transit of people from Wuhan to the rest of China. The geographic flow of people anticipated the subsequent location, intensity, and timing of outbreaks in the rest of China.
29 April
Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS-CoV-2 Infection in Residents of a Large Homeless Shelter in Boston. JAMA. 2020 Apr 27. PubMed: https://pubmed.gov/32338732. Full-text: https://doi.org/10.1001/jama.2020.6887
Between March 28, 2020, and April 1, 2020, authorities became aware of a few cases in a single large homeless shelter in Boston, prompting SARS-CoV-2 testing of all remaining shelter residents. In total, 147/408 (36%) were positive. Of note, 88% had no symptoms and no fever at the time of diagnosis.
28 April
Oliver N, Lepri B, Sterely H. Mobile phone data for informing public health actions across the COVID-19 pandemic life cycle. Science Advances 27 Apr 2020. Full-Text: https://doi.org/10.1126/sciadv.abc0764
This brief review outlines the ways in which different types of mobile phone data can help to better target and design measures to contain and slow the spread of the COVID-19 pandemic.
Bi Q, Wu Y, Mei S, et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Inf Dis. April 27, 2020. Full-Text: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30287-5/fulltext l (Important)
This important analysis of 391 early SARS-CoV-2 cases and their close contacts in Shenzhen, China, provides insight into the natural history and transmission. This work further supports a short incubation period (4–6 days). Notably, 5% took 14 days or more to develop symptoms. In multiple conditional logistic regression analysis of contact types, household contact (OR 6.3; 95% CI 1.5–26.3) and travelling together (OR 7.1; 1.4–34.9) were significantly associated with infection. The secondary attack rate was relatively low with 11·2% (95% CI 9·1–13·8) among household contacts and was similar across all age categories. However, this could be considered an underestimate, since transmission chains were cut short: index cases detected by symptom-based surveillance were rapidly isolated outside of the home.
Nie X, Fan L, Mu G, et al. Epidemiological characteristics and incubation period of 7,015 confirmed cases with Coronavirus Disease 2019 outside Hubei Province in China. J Inf Dis, 27 April 2020. Full-text: https://doi.org/10.1093/infdis/jiaa211
Huge study from China. Based on 2,907 confirmed cases, the median incubation period was 5 days, and more than 95% of cases had an incubation period of less than 13 days. From January 23, the incubation period among imported confirmed cases outside Hubei Province showed a gradual upward trend, but this trend was not obvious in non-imported cases.
27 April
Pearce N, Vandenbroucke JP, VanderWeele TJ, Greenland S. Accurate Statistics on COVID-19 Are Essential for Policy Guidance and Decisions. Am J Public Health. 2020 Apr 23:e1-e3. PubMed: https://pubmed.gov/32324422. Full-text: https://doi.org/10.2105/AJPH.2020.305708
Review of key epidemiological concepts and discussion of some of the preventable methodologic errors.
Mosites E, Parker EM, Clarke KE, et al. Assessment of SARS-CoV-2 Infection Prevalence in Homeless Shelters — Four U.S. Cities, March 27–April 15, 2020. MMWR, Early Release / April 22, 2020 / 69. Full-text: https://www.cdc.gov/mmwr/volumes/69/wr/mm6917e1.htm?s_cid=mm6917e1_w
Outbreaks in homeless shelters. If you test more than one person to be PCR positive, you already have many positive cases. Overall, 1,192 residents and 313 staff members were tested in 19 shelters from 4 US cities. When testing followed identification of a cluster, high proportions of positive tests were found, ranging from 16-66%. Testing in shelters where only one or no previous case had been identified found low prevalence (1-5%).
Arias-Reyes C, Zubieta-DeUrioste N, Poma-Machicao L, et al. Does the pathogenesis of SAR-CoV-2 virus decrease at high-altitude? Respir Physiol Neurobiol. 2020 Apr 22:103443. PubMed: https://pubmed.gov/32333993. Full-text: https://doi.org/10.1016/j.resp.2020.103443
Interesting idea. Epidemiological data from Tibet, Bolivia and Ecuador suggest that COVID-19 infection is decreased in populations living at an altitude of above 3,000 m. Highland inhabitants may be less susceptible to SARS-CoV-2 virus infection due to physiological acclimatization to hypoxia. High-altitude environmental factors may contribute to reduce the virulence of SARS-CoV-2. But can we be sure? The methods section of this paper contains one sentence. And the fact that the virus was written incorrectly even in the title, does not enhance credibility.
26 April
Chinazzi M, Davis JT, Ajelli M, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020 Apr 24;368(6489):395-400. PubMed: https://pubmed.gov/32144116. Full-text: https://doi.org/10.1126/science.aba9757
Complex transmission models, using epidemiological data from China. The authors concluded that the travel quarantine introduced in Wuhan on 23 January 2020 only delayed epidemic progression by 3 to 5 days within China, but international travel restrictions did help slow spread elsewhere by nearly 80% in the world until mid-February. The results suggest that even sustained 90% travel restrictions to and from mainland China only modestly affect the epidemic trajectory. Early detection, hand washing, self-isolation, and household quarantine will likely be more effective.
25 April
Gatto M, Bertuzzo E, Mari L, et al. Spread and dynamics of the COVID-19 epidemic in Italy: Effects of emergency containment measures. Proc Natl Acad Sci USA. 2020 Apr 23. PubMed: https://pubmed.gov/32327608. Full-text: https://doi.org/10.1073/pnas.2004978117
Complex models from Italy, quantifying the effect of local containment measures. The bottom line: the sequence of restrictions posed to mobility and human-to-human interactions have reduced transmission by 45% (42 to 49%). Models unquestionably support strong governmental decisions like those made in Italy.
24 April
Giordano G, Blanchini F, Bruno R, et al. Modelling the COVID-19 epidemic and implementation of population-wide interventions in Italy. Nat Med. 2020 Apr 22. PubMed: https://pubmed.gov/32322102. Full-text: https://doi.org/10.1038/s41591-020-0883-7
Interesting new model that predicts the course of the epidemic, considering eight stages of infection: susceptible (S), infected (I), diagnosed (D), ailing (A), recognized (R), threatened (T), healed (H) and extinct (E), collectively termed SIDARTHE. The model discriminates between infected individuals depending on whether they have been diagnosed and on the severity of their symptoms. Authors demonstrate that restrictive social-distancing measures will need to be combined with widespread testing and contact tracing to end the ongoing pandemic.
Peto J, Alwan NA, Godfrey KM, et al. Universal weekly testing as the UK COVID-19 lockdown exit strategy. Lancet. 2020 Apr 20. PubMed: https://pubmed.gov/32325027. Full-text: https://doi.org/10.1016/S0140-6736(20)30936-3
They have a dream: These UK researchers recommend the evaluation of weekly antigen testing of the whole population after lockdown. As they say, “a voluntary Dunkirk spirit” would be the only way for 10 million tests to be done daily.
23 April
Jiang XL, Zhang XL, Zhao XN, et al. Transmission potential of asymptomatic and paucisymptomatic SARS-CoV-2 infections: a three-family cluster study in China. J Infect Dis. 2020 Apr 22. PubMed: https://pubmed.gov/32319519. Full-text: https://doi.org/10.1093/infdis/jiaa206
Detailed cluster analysis, confirming that transmission by individuals with asymptomatic or paucisymptomatic infections is possible. An asymptomatic mother transmitted the virus to her son, and a paucisymptomatic father transmitted the virus to his three-month-old daughter. SARS-CoV-2 was detected in the environment of one household.
22 April
Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020 Apr 17. PubMed: https://pubmed.gov/32311320. Full-text: https://doi.org/10.1016/S2468-2667(20)30090-6
Detailed paper from Hong Kong modeling the effects of non-pharmaceutical interventions (NPIs, including border restrictions, quarantine and isolation, distancing, and changes in population behaviour). NPIs were associated with reduced transmission of COVID-19 and were also likely to have substantially reduced influenza transmission. Findings strongly suggest that social distancing and population behavioural changes – that have a social and economic impact that is less disruptive than a total lockdown – can meaningfully control COVID-19.
Wu X, Fu B, Chen L, Feng Y. Serological tests facilitate identification of asymptomatic SARS-CoV-2 infection in Wuhan, China. J Med Virol. 2020 Apr 20. PubMed: https://pubmed.gov/32311142. Full-text: https://doi.org/10.1002/jmv.25904
Forget herd immunity! Overall prevalence is still incredibly low. Even in hotspots like Wuhan! From April 3 to 15, SARS-CoV-2-specific IgG positive rate among 1,021 people applying for a permission to resume travel, only 98 (9.60%) were IgG positive and IgM and NAT (SARS‐CoV‐2 nucleic acid test) negative.
20 April
Normile D. ‘Suppress and lift’: Hong Kong and Singapore say they have a coronavirus strategy that works. Science Mag Apr 13, 2020. Full-text https://www.sciencemag.org/news/2020/04/suppress-and-lift-hong-kong-and-singapore-say-they-have-coronavirus-strategy-works#
The bottom line: the tighter you control the infected, the less restriction you have to impose on the uninfected. With this strategy, Hong Kong and Singapore are very successful. But look at the controls: hospitalizing all those who test positive, regardless of whether they have symptoms, two weeks of self-quarantine to all close contacts, electronic wristbands, etc. You want to see where the infected people in Hong Kong are? You’ll find them here: https://chp-dashboard.geodata.gov.hk/covid-19/en.html
Cheng KK, Lam TH, Leung CC. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. Lancet. 2020 Apr 16. PubMed: https://pubmed.gov/32305074. Full-text: https://doi.org/10.1016/S0140-6736(20)30918-1
The authors review current recommendations and conclude that mass masking for source control is a useful and low-cost adjunct to social distancing and hand hygiene, shifting the focus from self-protection to altruism, actively involving every citizen, and is a symbol of social solidarity in the global response to the pandemic.
19 April
Nickbakhsh S, Ho A, Marques DFP, McMenamin J, Gunson RN, Murcia PR. Epidemiology of seasonal coronaviruses: Establishing the context for COVID-19 emergence. J Infect Dis. 2020 Apr 15. PubMed: https://pubmed.gov/32296837. Full-text: https://doi.org/10.1093/infdis/jiaa185 l (Important)
Interesting and incredibly diligent work on seasonal coronaviruses (sCoVs) and other co-circulating viruses over a thirteen years period in Western Scotland, UK. Different sCoVs were detected in 4.0% (2,958/74,519) of tested patients overall, contributing to 10.7% of all respiratory virus detections. All were winter pathogens, on average peaking between January and March, alongside influenza viruses and RSV. However, there were notable variations between sCoV types and between years. A potential for cross-protective immunity was also seen between some subtypes.
18 April
CDC Covid Response Team. Characteristics of Health Care Personnel with COVID-19 – United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020 Apr 17;69(15):477-481. PubMed: https://pubmed.gov/32298247. Full-text: https://doi.org/10.15585/mmwr.mm6915e6
During February 12-April 9, among 315,531 COVID-19 cases reported to CDC, 49,370 (16%) included data on whether the patient was a health care worker (HCW). Detailed data were available on 8,945 of these HCW. Most HCW (90%) were not hospitalized; however, severe outcomes, including 27 deaths, occurred across all age groups. ICU admission and death were observed in 2.1–4.9% and 0.3-0.6%, respectively. These rates were markedly higher in HCW older than 65 years, with 6.9-16.0 % and 2.0-4.2%.
Anfinrud P, Stadnytskyi V, Bax CE, Bax A. Visualizing speech-generated oral fluid droplets with laser light scattering. N Engl J Med. https://doi.org/10.1056/NEJMc2007800.
You remember Depeche Mode’s hit ‘Enjoy the Silence’? Then look at this video, a person saying “stay healthy”, a laser light-scattering experiment in which speech-generated droplets and their trajectories were visualized. The louder the speech, the higher the numbers of flashes. The number of flashes was highest when the “th” sound in the word “healthy” was pronounced. Depeche Mode were right: “Words are very unnecessary/They can only do harm”.
Meselson M. Droplets and Aerosols in the Transmission of SARS-CoV-2. N Engl J Med. 2020 Apr 15. PubMed: https://pubmed.gov/32294374. Full-text: https://doi.org/10.1056/NEJMc2009324
These authors emphasize that breathing and talking produce even smaller and much more numerous particles, known as aerosol particles, than those visualized in the (above mentioned) laser experiment. They recommend wearing a suitable mask whenever it is thought that infected persons may be nearby and of providing adequate ventilation of enclosed spaces where such persons are known to be or may recently have been.
17 April
Szarpak L, Smereka J, Filipiak KJ, Ladny JR, Jaguszewski M. Cloth masks versus medical masks for COVID-19 protection. Cardiol J. 2020 Apr 14. PubMed: https://pubmed.gov/32285928. Full-text: https://doi.org/10.5603/CJ.a2020.0054
Some critical thoughts on the use of cloth masks. The physical properties of a cloth mask, reuse, the frequency and effectiveness of cleaning, and increased moisture retention, may potentially increase the infection risk.
15 April
Gudbjartsson DF, Helgason A, Jonsson H, et al. Spread of SARS-CoV-2 in the Icelandic Population. N Engl J Med. 2020 Apr 14. PubMed: https://pubmed.gov/32289214. Full-text: https://doi.org/10.1056/NEJMoa2006100
SARS-CoV-2 in Iceland. As of April 4, a total of 1,221 of 9,199 tested persons (13.3%) were positive. Why is this of interest? Because the country serves as a perfect epidemiological model. Key findings: The percentage of participants who tested positive in population screening remained stable (0.8%) in March, and the infection rates in two screening groups (recruited through open invitation and through random sampling) were not substantially different. Notably, 43% of the participants who tested positive reported having no symptoms.
Stone TE, Kunaviktikul W, Omura M, Petrini M. Editorial: Facemasks and the Covid 19 pandemic: What advice should health professionals be giving the general public about the wearing of facemasks? Nurs Health Sci. 2020 Apr 12. PubMed: https://pubmed.gov/32279450. Full-text: https://doi.org/10.1111/nhs.12724
Bottom line of this editorial (addressed to nurses): surgical facemasks by the general public is not recommended unless you are looking after a sick person in a household setting or are suffering from an illness. Far more effective is handwashing and maintaining a safe distance from other people.
Perc M, Miksić NG, Slavinec M et al. Forecasting COVID-19. Front. Phys., 08 April 2020 | https://doi.org/10.3389/fphy.2020.00127
Forecasts obtained with a simple iteration method that only needs the daily values of confirmed cases as input. The method takes into account expected recoveries and deaths, and it determines maximally allowed daily growth rates that lead away from exponential increase toward stable and declining numbers. Keeping the daily growth rates to below 5% is an important target for a promising outlook.
14 April
van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020 Mar 17. PubMed: https://pubmed.gov/32182409. Full-text: https://doi.org/10.1056/NEJMc2004973
This important work was published a few weeks ago. Today, no less than 6 correspondence letters mainly discuss airborne transmission and viability of SARS-CoV-2 in aerosols. The bottom line: viability was investigated under experimental conditions and should not be used to draw conclusions about airborne transmission. However, according to the authors, aerosol-generating medical procedures should be examined as well as decontamination techniques.
Sutton D, Fuchs K, D´Alton M, Goffman D. Universal Screening for SARS-CoV-2 in Women Admitted for Delivery. N Engl J Med. 2020 Apr 13. PubMed: https://pubmed.gov/32283004. Full-text: https://doi.org/10.1056/NEJMc2009316
Between March 22 and April 4, 2020, all pregnant women who delivered infants were tested in a hospital located on the northern tip of Manhattan, New York City. Nasopharyngeal swabs obtained from 210 asymptomatic women were positive in 29 (13.7%). All four women with symptoms of COVID-19 on admission were positive. In other words: 29/33 women were asymptomatic.
Kong WH, Li Y, Peng MW, et al. SARS-CoV-2 detection in patients with influenza-like illness. Nat Microbiol. 2020 Apr 7. PubMed: https://pubmed.gov/32265517. Full-text: https://doi.org/10.1038/s41564-020-0713-1
Re-analysing 640 throat swabs collected from patients in Wuhan with influenza-like-illness from 6 October 2019 to 21 January 2020, the authors found 9 to be positive for SARS-CoV-2. The onset date of the earliest case was 4 January 2020, one week after the outbreak was reported by hospitals.
13 April
Danis K, Epaulard O, Benet T, et al. Cluster of coronavirus disease 2019 (Covid-19) in the French Alps, 2020. Clin Infect Dis. 2020 Apr 11. PubMed: https://pubmed.gov/32277759. Full-text: https://doi.org/10.1093/cid/ciaa424
Some clusters are described, including a 9-yr-old child who attended three different schools (why 3 is not described) and one ski class while symptomatic. Coinfected with both picornavirus + influenza A(H1N1), the child transmitted only these viruses to others but not SARS-CoV-2, suggesting that these viruses are more easily transmitted than SARS-CoV-2.
Asadi S, Bouvier N, Wexler AS, Ristenpart WD. The coronavirus pandemic and aerosols: Does COVID-19 transmit via expiratory particles? Aerosol Sci Technol. 2020 Apr 3;0(0):1-4. PubMed: https://pubmed.gov/32308568. Full-text: https://doi.org/10.1080/02786826.2020.1749229. eCollection 2020
Why is SARS-CoV-2 so highly transmissible? This interesting overview describes current knowledge of airborne transmission. It’s not only the “droplet spray”, typically greater than 5 µm in diameter. Alternatively, a susceptible person can inhale microscopic aerosol particles consisting of the residual solid components of evaporated respiratory droplets, which are tiny enough to remain airborne for hours. The authors conclude that speech plausibly serves as an underrecognized transmission mechanism: “it is up to ‘aerosol scientists’ to provide the technology and hard data to either corroborate or reject that.” So please, get on the scene, aerosol scientists on this planet!
12 April
Guo ZD, Wang ZY, Zhang SF, et al. Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020. Emerg Infect Dis. 2020 Apr 10;26(7). PubMed: https://pubmed.gov/32275497. Full-text: https://doi.org/10.3201/eid2607.200885 l (Important)
In hospitals, the virus is everywhere. SARS-CoV-2 was widely distributed in the air and on object surfaces in both the intensive care units and general wards, implying a potentially high infection risk for medical staff. Contamination was greater in ICU. Virus was found on floors, computer mice, trash cans, and sickbed handrails and was detected in air approximately 4 m from patients.
Rossman H, Keshet A, Shilo S, et al. A framework for identifying regional outbreak and spread of COVID-19 from one-minute population-wide surveys. Nat Med. 2020 Apr 9. PubMed: https://pubmed.gov/32273611. Full-text: https://doi.org/10.1038/s41591-020-0857-9
Coronavirus infection spreads in clusters, and early identification of these clusters is critical for slowing down the spread of the virus. Short daily population-wide online surveys that assess the development of symptoms could serve as a strategic and valuable tools for identifying such clusters and informing epidemiologists, public health officials and policymakers.
10 April
Stafford N. Covid-19: Why Germany´s case fatality rate seems so low. BMJ. 2020 Apr 7;369:m1395. PubMed: https://pubmed.gov/32265194. Full-text: https://doi.org/10.1136/bmj.m1395
Guess why? It’s probably testing and nothing else. The more people with no or mild symptoms you test, the lower the fatality rate. Reliable PCR methods are reported through the end of January. In Germany’s public health system, testing is not restricted to a central laboratory as in many other nations but can be conducted at quality-controlled laboratories throughout the country. Within a few weeks, overall capacity reached half a million PCR tests a week. The same low fatality rate is seen in South Korea, another country with high testing rates.
Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020 Apr 8;4:CD013574. PubMed: https://pubmed.gov/32267544. Full-text: https://doi.org/10.1002/14651858.CD013574
A word from Cochrane. Current evidence for COVID-19 “is limited”. However, findings “consistently indicate that quarantine is important in reducing incidence and mortality”. In order to maintain the best possible balance of measures, “decision makers must constantly monitor the outbreak situation and the impact of the measures implemented”. Well.
8 April
Bae S, Kim MC, Kim JY, et al. Effectiveness of Surgical and Cotton Masks in Blocking SARS-CoV-2: A Controlled Comparison in 4 Patients. Ann Intern Med. 2020 Apr 6. PubMed: https://pubmed.gov/32251511. Full-text: https://doi.org/10.7326/M20-1342
Very small study, but both surgical and cotton masks appear to be ineffective in preventing the virus dissemination from the coughs of patients with COVID-19 to the environment and external mask surface.
6 April
Klompas M, Morris CA, Sinclair J, Pearson M, Shenoy ES. Universal Masking in Hospitals in the Covid-19 Era. N Engl J Med. 2020 Apr 1. PubMed: https://pubmed.gov/32237672. Full-text: https://doi.org/10.1056/NEJMp2006372
Thoughts on universal masking in hospitals. Pros and cons. Bottom line: The main value is probably psychological: giving health care workers the confidence to absorb and implement prevention practices.
Tian H, Liu Y, Li Y, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020 Mar 31. PubMed: https://pubmed.gov/32234804. Full-text: https://doi.org/10.1126/science.abb6105
“All models are wrong, but some are useful”, statistician George Box supposedly once said. This model shows how non-pharmaceutical measures have worked in China. Without the Wuhan travel ban, there would have been 744,000 cases by February 19, day 50 of the epidemic. With the Wuhan travel ban alone, the number of cases would have decreased to 202,000. Other control measures such as the national emergency response, together with the travel ban, limited the number of cases, 96% fewer than expected in the absence of interventions.
Normile D. As normalcy returns, can China keep COVID-19 at bay? Science. 2020 Apr 3;368(6486):18-19. PubMed: https://pubmed.gov/32241931. Full-text: https://doi.org/10.1126/science.368.6486.18
China is now addressing an issue every country and location in the world will eventually (hopefully) face: how to normalize and restore societal activities, while at the same time minimizing disease-related dangers from the outbreak.
Ghinai I, McPherson TD, Hunter JC, et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. 2020 Apr 4;395(10230):1137-1144. PubMed: https://pubmed.gov/32178768. Full-text: https://doi.org/10.1016/S0140-6736(20)30607-3
Infection of health-care workers (HCWs) is not inevitable! A female in her 60s who travelled to Wuhan on Dec 25, 2019, and returned to Illinois on Jan 13, 2020, transmitted the infection to her husband. Although both were hospitalised in the same facility and shared hundreds (n = 348) of contacts with HCWs, nobody else became infected, supporting recommendations regarding appropriate infection control.
5 April
Scott SE, Zabel K, Collins J, et al. First Mildly Ill, Non-Hospitalized Case of Coronavirus Disease 2019 (COVID-19) Without Viral Transmission in the United States — Maricopa County, Arizona, 2020. Clinical Infectious Diseases 2020, 02 April, ciaa374, https://doi.org/10.1093/cid/ciaa374
Is symptom severity a proxy for infectivity? Case report of a patient with mild illness and positive tests for up to 18 days after diagnosis, without evidence of transmission to 16 close contacts, among them 10 high-risk contacts.
Lu J, Gu J, Li K, et al. COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020. Emerg Infect Dis. 2020 Apr 2;26(7). PubMed: https://pubmed.gov/32240078. Full-text: https://doi.org/10.3201/eid2607.200764
Outbreak in a restaurant. The distances between index patient and persons at other tables were all > 1 m, suggesting that droplet transmission was prompted by air-conditioned ventilation.
Kwon SY, Kim EJ, Jung YS, Jang JS, Cho NS. Post-donation COVID-19 identification in blood donors. Vox Sang. 2020 Apr 2. PubMed: https://pubmed.gov/32240537. Full-text: https://doi.org/10.1111/vox.12925
Korean study of seven asymptomatic blood donors who were later identified as COVID-19 confirmed cases. None out of 9 recipients of platelets or red blood cell transfusions tested positive for SARS-CoV-2 RNA. Transfusion transmission is unlikely.
Chang L, Zhao L, Gong H, Wang L, Wang L. Severe Acute Respiratory Syndrome Coronavirus 2 RNA Detected in Blood Donations. Emerg Infect Dis. 2020 Apr 3;26(7). PubMed: https://pubmed.gov/32243255. Full-text: https://doi.org/10.3201/eid2607.200839
With screening of 2,430 donations in real-time, including 1,656 platelet and 774 whole blood donations from Wuhan, the authors found plasma samples positive for viral RNA from 4 asymptomatic donors. It remains unclear whether detectable RNA signifies infectivity.
4 April
Ferretti L, Wymant C, Kendall M, et al. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science 31 Mar 2020. https://doi.org/10.1126/science.abb6936
Using an analytically solvable model, authors show that viral spread is too fast to be contained by manual contact tracing. Spread could be controlled if this process was faster, more efficient and happened at scale. A contact-tracing app that builds a memory of proximity contacts and immediately notifies contacts of positive cases can achieve epidemic control if used by enough people, without need for lockdowns.
Flaxman S, Mishra S, Gandy A. Estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries. March 30. https://doi.org/10.25561/77731
Infection-control measures such as national lockdowns in many European countries are reducing the spread of coronavirus. Across 11 countries, between 21,000 and 120,000 deaths were probably avoided by the end of March, according to a model by a group at Imperial College London.
Leung NHL, Chu DKW, Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020 May;26(5):676-680. PubMed: https://pubmed.gov/32371934. Full-text: https://doi.org/10.1038/s41591-020-0843-2 ll (Outstanding)
Do face masks work? Yes, but it depends. This important study from Hong Kong (performed 2013-16) quantified virus in respiratory droplets and aerosols in exhaled breath. In total, 111 participants (infected with seasonal coronavirus, influenza or rhinovirus) were randomized to wear (or not) a simple surgical face mask. Results suggested that masks could be used by ill people to reduce onward transmission. But note the small numbers: in respiratory droplets, seasonal coronavirus was found in 0/11 droplets (aerosols: 0/11) from participants wearing face masks, compared to 3/10 (aerosols: 4/10) without masks. Influenza viruses were detected in 1/27 (aerosols 6/27!) with face masks, compared to 6/23 (8/23) without. For rhinovirus, there were no significant differences at all. Of note, authors also identified virus in some participants who did not cough at all during the 30-min exhaled breath collection, suggesting droplet and aerosol routes of transmission from individuals with no obvious signs or symptoms.
Chin AW, Chu JT, Perera MR, et al. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe 2020, April 02. Full-text: https://doi.org/10.1016/S2666-5247(20)30003-3 l (Important)
Don’t put your masks in the fridge for recycling! Heating is probably better. This important work shows that the virus was highly stable at 4°C (almost no reduction on day 14) but sensitive to heat (70° C: inactivation 5 min, 56°: 30 min, 37°: 2 days). It also depends on the surface: No infectious virus could be recovered from printing and tissue papers after 3 hours, from treated wood and cloth on day 2, from glass and banknotes on day 4, stainless steel and plastic on day 7. Strikingly, a detectable level of infectious virus (∼0·1% of the original inoculum) could still be present on the outer layer of a surgical mask on day 7.
3 April
Luo C, Yao L, Zhang L, et al. Possible Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in a Public Bath Center in Huai´an, Jiangsu Province, China. JAMA Netw Open. 2020 Mar 2;3(3):e204583. PubMed: https://pubmed.gov/32227177. Full-text: https://doi.org/10.1001/jamanetworkopen.2020.4583
A cluster-spreading event in Huai’an, China, in which a patient may have transmitted the virus to 8 other individuals via bathing in a public bath center (sauna, bath, 25 to 41° C and humidity of approximately 60%). Transmissibility appears not to be reduced in warm and humid conditions.
Cereda D, Tirani M, Rovida F, et al. The early phase of the COVID-19 outbreak in Lombardy, Italy. Preprint. Full-text: https://arxiv.org/abs/2003.09320
Still looking for patient zero in Italy (not found). However, this important study of 6,000 laboratory-confirmed cases tracks how the outbreak unfolded in the region. By the time the first case was detected, the virus had already spread (since January) to most towns and cities in southern Lombardy.
2 April
Chan KH, Yuen KY. COVID-19 epidemic: disentangling the re-emerging controversy about medical face masks from an epidemiological perspective. Int J Epidem March 31, 2020. dyaa044. Full-text: https://doi.org/10.1093/ije/dyaa044
Review of data and inconsistencies in official guidelines and expert opinions about face masks, confusing both the public and health care professionals. Still wondering, after reading this review.
Dudly JP, Lee NT. Disparities in Age-Specific Morbidity and Mortality from SARS-CoV-2 in China and the Republic of Korea. Clin Inf Dis 2020, March 31. Full-text: https://doi.org/10.1093/cid/ciaa354
Morbidity in China exhibited a Gaussian distribution (peak 50-59 years), while morbidity in ROK had a bimodal distribution (peak 20-29 years). Careless youth? Authors speculate that this was possibly due to differences in public health intervention practices and age-related sociocultural factors (lower rates of compliance among younger people with social distancing and self-quarantine recommendations).
Patrick GT, Whittaker C, Watson O, et al. The Global Impact of COVID-19 and Strategies for Mitigation and Suppression. Imperial College London 2020, published March 26. Full-text: https://doi.org/10.25561/77735.
Elegant models illustrating the potential impact of the COVID-19 pandemic globally and highlighting the challenging decisions faced by governments. In the absence of interventions, COVID-19 would have resulted in 7.0 billion infections and 40 million deaths globally this year. Mitigation strategies focussing on shielding the elderly (60% reduction in social contacts) and slowing but not interrupting transmission (40% reduction) could reduce this burden by half, saving 20 million lives.
Wells CR, Sah P, Moghadas SM, et al. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci U S A. 2020 Mar 13. PubMed: https://pubmed.gov/32170017. Full-text: https://doi.org/10.1073/pnas.2002616117
Complex epidemiological models, showing that border controls, airport screening and travel restrictions likely slowed the rate of exportation from mainland China to other countries, but were insufficient to contain the global spread of COVID-19. Rapid contact tracing remains essential.
31 March
Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020 Apr;8(4):e488-e496. PubMed: https://pubmed.gov/32119825. Fulltext: https://doi.org/10.1016/S2214-109X(20)30074-7
Excellent work with implications for future outbreaks and the time after lockdown. Using a stochastic transmission model, contact tracing and isolation of cases was sufficient to control a new outbreak.