22 November
Paccou J, Lenne X, Ficheur G, et al. Analysis of Hip Fractures in France During the First COVID-19 Lockdown in Spring 2020. JAMA Netw Open November 17, 2021;4(11):e2134972. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2786201?resultClick=1
Hospitalizations for hip fractures in France decreased by 11% during the first nationwide lockdown.
19 November
Harris TG, Jaszi E, Lamb MR, et al. Effects of the COVID-19 Pandemic on HIV Services: Findings from 11 Sub-Saharan African Countries. Clinical Infectious Diseases November 15, 2021, ciab951, https://doi.org/10.1093/cid/ciab951
Far less damage than expected. While initial declines were observed, rebound was brisk as the pandemic progressed, with increases noted in the number tested, whether newly-initiated HIV or currently on ART, VL testing, and VLS throughout the period, demonstrating substantial HIV program resilience in the face of the COVID-19 crisis.
18 November
Asch DA, Buresh J, Allison KC, et al. Trends in US Patients Receiving Care for Eating Disorders and Other Common Behavioral Health Conditions Before and During the COVID-19 Pandemic. JAMA Netw Open November 16, 2021;4(11):e2134913. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2786185?resultClick=1
Inpatient stays for eating disorders on the rise. This increase was around two-fold and was seen across anorexia nervosa, bulimia nervosa, and other and unspecified eating disorders.
14 November
Peng Y, Wu P, Schartup AT, et al. Plastic waste release caused by COVID-19 and its fate in the global ocean. PNAS November 23, 2021 118 (47) e2111530118; https://doi.org/10.1073/pnas.2111530118
This work shows that more than eight million tons of pandemic-associated plastic waste have been generated globally, with more than 25,000 tons entering the global ocean. Most of the plastic is from medical waste generated by hospitals that dwarfs the contribution from personal protection equipment and online-shopping package material.
12 November
Grunert KG, Janssen M, Nyland Christensen R, et al. “Corona Cooking”: The interrelation between emotional response to the first lockdown during the COVID-19 pandemic and cooking attitudes and behaviour in Denmark. Food Qual Prefer. 2022 Mar;96:104425. PubMed: https://pubmed.gov/34629761. Full text: https://doi.org/10.1016/j.foodqual.2021.104425
Believe it or not. It appears that the pandemic helped some people rediscover their liking for home cooking and meals at home.
1 November
Orhant ER, Chapellier JF, Carling C. Injury rates and patterns in French male professional soccer clubs: a comparison between a regular season and a season in the COVID-19 pandemic. Res Sports Med 2021 October 27;1-11. https://pubmed.ncbi.nlm.nih.gov/34706601/
More good news for Joshua. In this national injury database, no differences in the incidence of match injuries affecting the ankle and knee regions were observed during the French 2020/2021 season. However, we urgently need more data to see whether this applies to other leagues.
Ghiani G, Roberto S, Mura R, et al. Body composition changes during the lockdown-restart transition due to the SARS-CoV-2 pandemic in a group of professional football players. J Sports Med Phys Fitness October 15, 2021. https://pubmed.ncbi.nlm.nih.gov/34651614/
And even more. This groundbreaking study evaluated the body composition of 18 male football players from an Italian Serie A team by bioelectrical impedance. It is encouraging to see that after lockdown, no changes in body mass, body mass index, fat mass, fat-free mass, or total body water were seen.
25 October
Abraham JO, Mumma MA. Elevated wildlife-vehicle collision rates during the COVID-19 pandemic. Sci Rep October 15 11, 20391 (2021). https://doi.org/10.1038/s41598-021-99233-9
Increased wildlife road use offsets the effects of decreased traffic volume on vehicle-wildlife collisions.
Asare S, Majmundar A, Islami F, et al. Changes in Cigarette Sales in the United States During the COVID-19 Pandemic. Ann Int Med, October 19, 2021. https://doi.org/10.7326/M21-3350 4
A monthly excess sale of 0.34 packs (95% CI: 0.25 to 0.44 packs) per capita.
15 October
Nogrady B. ‘I hope you die’: how the COVID pandemic unleashed attacks on scientists. Nature 2021, published 13 October. Full text: https://www.nature.com/articles/d41586-021-02741-x
“A survey by Nature of more than 300 scientists who have given media interviews about COVID-19 — many of whom had also commented about the pandemic on social media — has found wide experience of harassment or abuse; 15% said they had received death threats.” See also the Nature editorial: COVID scientists in the public eye need protection from threats. Nature 2021, published 13 October. Full text: https://www.nature.com/articles/d41586-021-02757-3
11 October
Cousien A, Acquaviva E, Kernéis S, Yazdanpanah Y, Delorme R. Temporal Trends in Suicide Attempts Among Children in the Decade Before and During the COVID-19 Pandemic in Paris, France. JAMA Netw Open. 2021 Oct 1;4(10):e2128611. PubMed: https://pubmed.gov/34618041. Full text: https://doi.org/10.1001/jamanetworkopen.2021.28611
The authors describe a dramatic increase in suicide attempts among children in late 2020 and early 2021 after the start of the COVID-19 pandemic in France. “This aberrant dynamic of suicide attempts was independent from its annual seasonality and its trend over the 10-year period.”
COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, published 8 October. Full text: https://doi.org/10.1016/S0140-6736(21)02143-7
A systematic review of major depressive disorder and anxiety disorders during the COVID-19 pandemic. Daily SARS-CoV-2 infection rates and reductions in human mobility were associated with increased prevalence of major depressive disorder. Females were more affected than males for major depressive disorder, and younger age groups were more affected than older age groups.
10 October
Das-Munshi J, Change CK, Bakolis I, et al. All-cause and cause-specific mortality in people with mental disorders and intellectual disabilities, before and during the COVID-19 pandemic: cohort study. Lancet Regional Health 2021, published 7 October. Full text: https://www.thelancet.com/journals/lanepe/article/PIIS2666-7762(21)00214-3/fulltext
Data from a prospective analysis of 167,122 people in the UK: “People with mental disorders and intellectual disabilities were at a greater risk of death relative to the general population before, during and after the first peak of COVID-19 deaths, with similar risks by ethnicity.” The authors conclude that the COVID-19 pandemic has exacerbated pre-existing health inequalities in people living with mental disorders and intellectual disabilities.
9 October
COVIDSurg Collaborative. Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Oncology 2021, published 5 October. Full text: https://doi.org/10.1016/S1470-2045(21)00493-9
Although surgery, the main modality of cure for solid cancers, was prioritized to continue during COVID-19 outbreaks, 2003 (10%) of 20,006 eligible patients did not receive surgery after a median follow-up of 23 weeks.
25 September
Agarwal S, Huang P, Luo C, et al. Assessment of Online Food Ordering and Delivery in Singapore During the COVID-19 Pandemic. JAMA Netw Open September 23, 2021;4(9):e2126466. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2784439?resultClick=1
Less vegetables, more junk food: using a data set of 42,495 real food orders, this study suggests an association with unhealthier eating habits during the COVID-19 lockdown. The probability that the order contained vegetables decreased by 15%, while the probability of an order in the barbecue/fried food or beverage category increased by 11% and 4%, respectively. Of note, changes in eating habits persisted after lockdown measures were removed.
Ray LC, Collins JP, Griffin PM, et al. Decreased Incidence of Infections Caused by Pathogens Transmitted Commonly Through Food During the COVID-19 Pandemic — Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2017–2020. MMWR Morb Mortal Wkly Rep 2021;70:1332–1336. https://www.cdc.gov/mmwr/volumes/70/wr/mm7038a4.htm?s_cid=mm7038a4_w
More junk food, but less infections: the 26% decrease in incidence of infections caused by pathogens transmitted commonly through food during 2020 was the largest single-year variation in incidence over the last 25 years in the US. Widespread public health interventions implemented to prevent SARS-CoV-2 transmission might have contributed to this decrease.
19 September
Peña PA, Jena A. Mass Shootings in the US During the COVID-19 Pandemic. JAMA Netw Open September 16, 2021;4(9):e2125388. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2784187?resultClick=1
Beautifully put. After arguing that “mass shootings are rare events with causes that are not well understood”, the authors analyzed 2985 (!) mass shootings in the US, involving 3185 people killed and 12,547 injured. Bottom line: mass shootings are on the increase, possibly indicating that mass murderers may also be stressed these days (well, has anyone suggested gun laws?)
6 September
Hawrilenko M, Krohus E, Tandon P, et al. The Association Between School Closures and Child Mental Health During COVID-19. JAMA Netw Open September 3, 2021; 4(9):e2124092. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2783714?resultClick=1
In this survey study of 2324 adults with at least 1 school-age child, a small association between school closures and worse child mental health outcomes was observed. Children from families with lower income experienced more mental health problems associated with school closures.
30 August
Jarnig G, Jaunig J, van Poppel MN, et al. Association of COVID-19 Mitigation Measures With Changes in Cardiorespiratory Fitness and Body Mass Index Among Children Aged 7 to 10 Years in Austria. JAMA Netw Open August 26, 2021; 4(8):e2121675. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2783511?resultClick=1
In this cohort study of Austrian children aged 7 to 10 years, fitness levels decreased and BMI increased from September 2019 to September 2020, most likely in association with COVID-19 mitigation measures. The proportion of overweight or obese children increased by 3.1% among girls and 4.5% among boys.
Nichter B, Hill ML, Na PJ, et al. Prevalence and Trends in Suicidal Behavior Among US Military Veterans During the COVID-19 Pandemic. JAMA Psychiatry. 2021; https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2783601?resultClick=1
Despite grim forecasts about the COVID-19 pandemic possibly creating a perfect storm for suicidal behavior, the prevalence of suicidality DID NOT increase among military veterans.
27 August
Burdzovic Andreas J, Scott Brunbirg G. Self-reported Mental and Physical Health Among Norwegian Adolescents Before and During the COVID-19 Pandemic. JAMA Netw Open August 24 2021;4(8):e2121934. doi:10.1001/jamanetworkopen.2021.21934
Most adolescents cope adequately with the pandemic conditions. However, they are at high risk becoming couch potatoes: this large cohort study including 2536 adolescents found that Norwegian adolescents starting high school during the COVID-19 year had lower odds of sports participation than their peers starting high school in preceding years, but no significant differences in depression symptoms, friendships, and physical health.
Ujiie M, Tsuzuki S, Nakamoto T, Iwamoto N. Resurgence of respiratory syncytial virus infections during COVID-19 pandemic, Tokyo, Japan. Emerg Infect Dis. 2021 Nov [date cited]. https://wwwnc.cdc.gov/eid/article/27/11/21-1565_article
As of July 2021, however, an unusually high number of respiratory syncytial virus infections were reported in Tokyo. This resurgence (the largest annual increase in cases since monitoring began in 2003) may have resulted from restarting social activities for children.
23 August
Brink J, Cullen P, Beek K, Peters SAE. Intimate Partner Violence during the Covid-19 pandemic in Western and Southern European countries. Eur J Public Health. 2021 Aug 18:ckab093. PubMed: https://pubmed.gov/34406373. Full text: https://doi.org/10.1093/eurpub/ckab093
“Six countries showed an increase in domestic violence reports (Austria, Belgium, France, Ireland, Spain, and the UK), two countries a drop (Italy and Portugal), two countries showed no change (the Netherlands and Switzerland), and one country did not provide comparative data (Germany).”
11 August
Kidman R. Use HIV’s lessons to help children orphaned by COVID-19. Nature 2021, published 9 August. Full text: https://www.nature.com/articles/d41586-021-02155-9
“Young people who have lost parents to the pandemic need urgent support and long-term study to avert the cascade of adversity that can follow. Decades of research into the HIV epidemic provide(s) a solid foundation.”
9 August
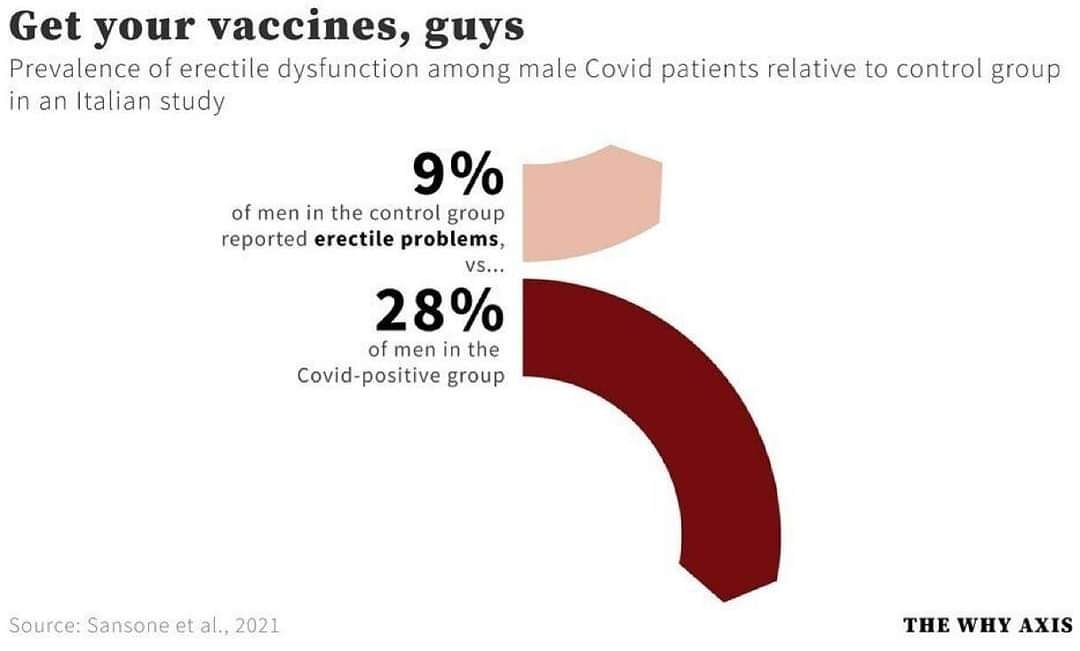
Sansone A, Mollaioli D, Ciocca G, et al. “Mask up to keep it up”: Preliminary evidence of the association between erectile dysfunction and COVID-19. Andrology. 2021 Jul;9(4):1053-1059. PubMed: https://pubmed.gov/33742540. Full text: https://onlinelibrary.wiley.com/doi/10.1111/andr.13003 | See also the informal discussion at https://theconversation.com/covid-19-could-cause-male-infertility-and-sexual-dysfunction-but-vaccines-do-not-164139
Erectile dysfunction (ED) could be a short‐ or long‐term complication of COVID‐19. In this analysis of 100 people (25 COVID‐positive and 75 COVID‐negative), the prevalence of ED was significantly higher in the COVID+ group (28% vs. 9.33%; p = 0.027).
2 August
Burki K. Tobacco industry capitalises on the COVID-19 pandemic. Lancet Resp Med 2021, published 29 July. Full text: https://doi.org/10.1016/S2213-2600(21)00361-1
“Ever since the tobacco industry started marketing its products, it has attempted to hitch them to key trends and events. Adverts during World War One associated tobacco with victory. The industry would subsequently deploy the rhetoric of the suffragette movement with the “torches of freedom” campaign. Virginia Slims introduced the tagline “you’ve come a long way, baby” in the late 1960s, playing on the feminist themes of the era. “Today, we see the industry paying influencers on social media to push e-cigarettes, which they claim are harmless and cool, when in fact the whole point is to get a new generation addicted to nicotine. (…) As soon as COVID-19 arrived, they recognized the opportunity that the pandemic presented.”
26 July
Bernstein AN, Talwar R, Handorf E, et al. Assessment of Prostate Cancer Treatment Among Black and White Patients During the COVID-19 Pandemic. JAMA Oncol. 2021 Jul 22. PubMed: https://pubmed.gov/34292311. Full-text: https://doi.org/10.1001/jamaoncol.2021.2755
During the initial phase of the pandemic only 1% of Black men underwent prostatectomy for untreated nonmetastatic prostate cancer, while 26% of White patients did. Before the pandemic, there was no difference in the rate of prostatectomy between the 2 races. Read also the comment by Vince R Jr. The Intersection of Societal Inequalities and Health Care: Lessons Learned From the COVID-19 Pandemic. JAMA Oncol. 2021 Jul 22. PubMed: https://pubmed.gov/34292296. Full-text: https://doi.org/10.1001/jamaoncol.2021.2750
25 July
Olsen SJ, Winn AK, Budd AP, et al. Changes in Influenza and Other Respiratory Virus Activity During the COVID-19 Pandemic – United States, 2020-2021. MMWR Morb Mortal Wkly Rep. 2021 Jul 23;70(29):1013-1019. PubMed: https://pubmed.gov/34292924. Full-text: https://doi.org/10.15585/mmwr.mm7029a1
Common human coronaviruses, parainfluenza viruses, and respiratory adenoviruses, etc. on the rise again. “Clinicians should be aware of increased circulation, sometimes off-season, of some respiratory viruses and consider multipathogen testing.”
23 July
Hillis SD, Unwin HJT, Chen Y, et al. Global minimum estimates of children affected by COVID-19-associated orphanhood and deaths of caregivers: a modelling study. Lancet 2021, published 20 July. Full text: https://doi.org/10.1016/S0140-6736(21)01253-8
From March 1, 2020, to April 30, 2021, more than one million children lost at least one parent or custodial grandparent.
See also the comment by Kentor RA, Thompson AL. Answering the call to support youth orphaned by COVID-19. Lancet 2021, published 20 July. Full text: Lancet 2021, published 20 July. Full text: https://doi.org/10.1016/S0140-6736(21)01253-8
20 July
Causey K, Fullman N, Sorensen RJD, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet 2021, published 14 July. Full text: https://doi.org/10.1016/S0140-6736(21)01337-4
In 2020, tens of millions of children missed DTP3, the third-dose of the diphtheria-tetanus-pertussis vaccine, and MCV1, the first-dose of a measles-containing vaccine.
See also the comment by Abbas K, Mogasale V. Disruptions to childhood immunisation due to the COVID-19 pandemic. Lancet 2021, published 14 July. Full text: https://doi.org/10.1016/S0140-6736(21)01418-5
18 July
Causey K, Fullman N, Sorensen RJ, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet July 14, 2021. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01337-4/fulltext
Routine immunization services faced stark challenges in 2020, with the COVID-19 pandemic causing the most widespread and largest global disruption in recent history. Although the latest coverage trajectories point towards recovery in some regions, a combination of lagging catch-up immunization services, continued SARS-CoV-2 transmission, and persistent gaps in vaccine coverage before the pandemic still left millions of children under-vaccinated or unvaccinated against preventable diseases at the end of 2020, and these gaps are likely to extend throughout 2021.
3 July
Pieh C, Plener PL, Probst T, et al. Assessment of Mental Health of High School Students During Social Distancing and Remote Schooling During the COVID-19 Pandemic in Austria. JAMA Netw Open June 28, 2021; 4(6):e2114866. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2781462?resultClick=1
This cross-sectional study suggests that the COVID-19 pandemic was associated with impaired mental health. The mental well-being and life satisfaction in adolescents in Austria were significantly lower in 2021 compared with 2018. However, owing to the online nature of the study, a self-selection bias toward higher participation of adolescents with a higher mental health burden may be possible.
30 June
Wilmers CC, Nisi AC, Ranc N, et al. COVID-19 suppression of human mobility releases mountain lions from a landscape of fear. Current Biology June 23, 2021DOI:https://doi.org/10.1016/j.cub.2021.06.050
One day, when humans will all be gone from earth, nature will quickly come out of its holes. Mountain lions first (according to this study where GPS collars were placed on six animals). Results: The drastic change in human behavior due to the Covid-19 pandemic had cascading effects on mountain lion habitat selection. Under normal circumstances, mountain lions strongly avoid urban areas. When human mobility declined by more than 50% during the Covid-19 associated lockdown, mountain lions relaxed their fear of the urban edge during the lockdown.
Wan WY, Thoon KC, Loo LH, et al. Trends in Respiratory Virus Infections During the COVID-19 Pandemic in Singapore, 2020. JAMA Netw Open June 28, 2021. 4(6):e2115973. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2781461?resultClick=1
A decrease in influenza was already seen following relatively modest control measures, including mask-wearing recommendations among only ill or symptomatic individuals. Influenza remained nearly absent for the remainder of 2020. International travel restrictions likely contributed to this. For enterovirus/rhinovirus and adenovirus, reductions were only seen after lockdown, and these viruses rebounded earlier than others. Continued mandatory mask wearing did not appear to prevent this.
24 June
Lepak AJ, Taylor LN, Stone CA, et al. Association of Changes in Seasonal Respiratory Virus Activity and Ambulatory Antibiotic Prescriptions With the COVID-19 Pandemic. JAMA Intern Med June 21, 2021. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2781312
This study from Wisconsin, US demonstrated a marked decrease in respiratory virus detection, with a concomitant 79% decline in ambulatory antibiotic prescribing rates for respiratory tract infections, during the COVID-19 pandemic.
Duffy E, Thomas M, Hills T, Ritchie S. The impacts of New Zealand’s COVID-19 epidemic response on community antibiotic use and hospitalisation for pneumonia, peritonsillar abscess and rheumatic fever. Lancet Regional Health July 01, 2021. https://www.thelancet.com/journals/lanwpc/article/PIIS2666-6065(21)00071-7/fulltext
Same findings from New Zealand. Antibiotic dispensing rates fell by 36%, suggesting that countries with high rates of antibiotic use could significantly reduce their use without an increase in morbidity.
22 June
Braunstein SL, Slutsker JS, Lazar R, et al. Epidemiology of reported HIV and other sexually transmitted infections during the COVID-19 pandemic, New York City. J Inf Dis Jun 16, 2021, jiab319, https://doi.org/10.1093/infdis/jiab319.
During NYC lockdown, the volume of positive HIV/STI tests, and diagnoses of HIV, chlamydia, gonorrhea, and syphilis declined substantially, reaching a nadir in April before rebounding.
20 June
Hunter RF, Garcia L, de Sa TH et al. Effect of COVID-19 response policies on walking behavior in US cities. Nat Commun 12 June 15, 2021, 3652. https://www.nature.com/articles/s41467-021-23937-9
Analyzing mobility data from mobile devices and area-level data to study the walking patterns of 1.62 million anonymous users in 10 metropolitan areas in the US, this study reveals dramatic declines in walking, particularly utilitarian walking, while recreational walking has recovered and even surpassed pre-pandemic levels.
14 June
Yard E, Radhakrishnan L, Ballesteros MF, et al. Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12–25 Years Before and During the COVID-19 Pandemic — United States, January 2019–May 2021. MMWR 11 June 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7024e1.htm?s_cid=mm7024e1_w
During February 21–March 20, 2021, suspected suicide attempt ED visits were 50.6% higher among girls aged 12–17 years than during the same period in 2019; among boys aged 12–17 years, suspected suicide attempt ED visits increased 3.7%.
Nivette AE, Zahnow R, Aguilar R et al. A global analysis of the impact of COVID-19 stay-at-home restrictions on crime. Nat Hum Behav June 2, 2021. https://doi.org/10.1038/s41562-021-01139-z
Crime largely decreased around the globe during COVID-19 stay-at-home orders, but with substantial variation across cities and types of crime. Property-based crimes decreased substantially, but homicide was relatively unchanged. Meta-regression results showed that more stringent restrictions over movement in public space were predictive of larger declines in crime.
7 June
Sout MJ, van de Ven CJ, Parekh VI, et al. Use of Electronic Medical Records to Estimate Changes in Pregnancy and Birth Rates During the COVID-19 Pandemic. JAMA Netw Open June 3, 2021;4(6):e2111621. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2780572?resultClick=1
In this cohort study from Michigan, a 14% reduction in pregnancy episode initiation was observed, probably due to a decrease in conceptions that followed the March 15 mandated COVID-19 pandemic societal shutdown. Prospective modeling of pregnancies currently suggests that a birth volume surge can be anticipated in summer 2021.
4 June
Solomon MD, Nguyen-Huynh M, Leong TK. Changes in Patterns of Hospital Visits for Acute Myocardial Infarction or Ischemic Stroke During COVID-19 Surges. JAMA June 2, 2021. https://jamanetwork.com/journals/jama/fullarticle/2780794?resultClick=1
In contrast to the initial COVID-19 surge during March / April 2020, no significant declines in AMI hospitalization or stroke alerts were observed during the largest and most recent surge from October 2020 to January 2021 in Kaiser Permanente, Northern California.
30 May
Bodilsen J, Nielsen PB, Søgaard M. Hospital admission and mortality rates for non-covid diseases in Denmark during covid-19 pandemic: nationwide population based cohort study. BMJ 25 May 2021, 373. https://www.bmj.com/content/373/bmj.n1135
Hospital admissions for all major non-COVID-19 disease groups were 30% and 22% lower during the two national lockdowns compared to previous years. Additionally, mortality rates were higher overall and for patients admitted to hospital with conditions such as respiratory diseases, cancer, pneumonia, and sepsis.
29 May
Brueggemann AB, Jansen van Rensburg MJ, Shaw D, et al. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digital Health, June 1, 2021. Volume 3, ISSUE 6, e360-e370 https://www.thelancet.com/journals/landig/article/PIIS2589-7500(21)00077-7/fulltext
In this large study including 27 laboratories from 26 countries and territories, all laboratories experienced a significant and sustained reduction in invasive diseases due to S. pneumoniae, H. influenzae, and N. meningitis in early 2020. By contrast, no significant changes in the incidence of invasive S. agalactiae infections were observed. The incidence of reported S. pneumoniae infections decreased by 68% at 4 weeks and 82% at 8 weeks following the week in which significant changes in population movements were recorded.
15 May
Carr J, Wright AK, Leelarathna L, et al. Impact of COVID-19 on diagnoses, monitoring, and mortality in people with type 2 diabetes in the UK. Lancet Diab Endocrin May 11, 2021. https://www.thelancet.com/journals/landia/article/PIIS2213-8587(21)00116-9/fulltext
In April 2020, the rate reduction of new diagnoses of type 2 diabetes in primary care practices in England was 0.70 when compared with 10-year historical trends. Older individuals (65 years and older), men, and people from deprived areas had the greatest reductions in diagnosis rates.
15 April
Pirkis J, John A, Shin S, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry April 13, 2021. https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(21)00091-2/fulltext
Was there an early effect of the COVID-19 pandemic on suicide rates around the world? Probably not. In high-income and upper-middle-income countries, suicide numbers have remained largely unchanged or declined in the early months of the pandemic compared with the expected levels based on the pre-pandemic period.
22 March
Adlhoch C, Mook P, Lamb F, et al. Very little influenza in the WHO European Region during the 2020/21 season, weeks 40 2020 to 8 2021. Eurosurveillance 18 March 2021, Volume 26, Issue 11. https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2021.26.11.2100221
Almost no flu this year. This 2020/21 influenza season is exceptional since the creation of the Global Influenza Surveillance and Response System (GISRS) network in 1952. Positivity was 0.1% (33/25,606) this season compared to an average positivity of 38% (14,966/39,407) between week 40 year X and week 8 the following year. Yes, this was statistically significant.
15 March
Li L, Neuroth LM, Valachovic E, et al. Association Between Changes in Social Distancing Policies in Ohio and Traffic Volume and Injuries, January Through July 2020. JAMA March 9, 2021;325(10):1003-100. https://jamanetwork.com/journals/jama/fullarticle/2777228
Better stay home, it’s better for everybody. Compared to 2019, the period between the stay-at-home order and retail reopening (March 23 through May 11, 2020) in Ohio saw 55% fewer motor vehicle crash involvements, 47% fewer injuries, 34% fewer severe/fatal injuries, and 44% lower traffic volume.
12 March
Maselli-Schoueri JH, Werneck de Carvalho LE, Affonso Fonseca FL, et al. Hospital Admissions Associated With Noncommunicable Diseases During the COVID-19 Outbreak in Brazil. JAMA Netw Open March 8, 2021; 4(3):e210799. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2777139 Reduction in hospital admissions for NCDs from January to June 2020 compared with the corresponding period in each of the 3 previous years in São Paulo, Brazil. Decrease was 68% for musculoskeletal diseases, 44% for metabolic diseases, 38% for CVDs, and 35% for neoplasms.
5 March
Knudsen AK, Stene-Larsen K, Gustavson K, et al. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: A population-based repeated cross-sectional analysis. Lancet Regional Health February 27, 2021. Volume 4, 100071, May 01, 2021DOI: https://doi.org/10.1016/j.lanepe.2021.100071
Credible data from Norway: except for a decrease in mental disorders in the first pandemic period, the findings suggest stable levels of mental disorders, suicidal ideation and suicide deaths during the first six months of the COVID-19 pandemic compared to pre-pandemic levels.
4 March
Shepherd JP, Moore SC, Long A, et al. Association Between COVID-19 Lockdown Measures and Emergency Department Visits for Violence-Related Injuries in Cardiff, Wales. JAMA March 2, 2021. 2021; 325(9):885-887. https://jamanetwork.com/journals/jama/article-abstract/2776868
Less violence during lockdown. In Cardiff, Wales, the average weekly number of violent injury admissions dropped from 28.4 to 16.5 during lockdown. There was also a 92% reduction in weapon use. This may reflect closure of city center pubs and clubs where most violence takes place. Cheers.
24 February
Ghafil C, Matsushima K, Henry R, et al. Trends in Trauma Admissions During the COVID-19 Pandemic in Los Angeles County, California. JAMA Netw Open. February 22, 2021;4(2):e211320. Full-text: https://doi.org/10.1001/jamanetworkopen.2021.1320
Less accidents (for a few weeks) but more gunshots? In this retrospective cohort study of 6777 trauma admissions in Los Angeles County from January 1 to June 7, 2020, overall volume transiently decreased but quickly returned to baseline. Mechanisms of injury were significantly different, with a steady increase in admissions for “penetrating” injuries (in other words: mainly gunshots).
23 February
Fong MW, Leung NHL, Cowling BJ, Wu P. Upper respiratory infections in schools and childcare centers reopening after COVID-19 dismissals, Hong Kong. Emerg Infect Dis, February 17, 2021 (May date cited). https://wwwnc.cdc.gov/eid/article/27/5/21-0277_article
A large number of outbreaks of acute upper respiratory tract infections (URTIs), likely rhinovirus infections, were identified in October–November 2020 in reopened primary schools, secondary schools, kindergartens, childcare centers, and nursery schools in Hong Kong; these outbreaks led to further territory-wide school dismissals for younger children. Increased susceptibility to rhinoviruses during prolonged school closures and dismissals for coronavirus disease and varying effectiveness of nonpharmaceutical interventions may have heightened transmission of cold-causing viruses when school attendance resumed.
8 February
Dorward J, Khubone T, Gate K, et al. The impact of the COVID-19 lockdown on HIV care in 65 South African primary care clinics: an interrupted time series analysis. Lancet HIV 2021, published 4 February. Full-text: https://doi.org/10.1016/S2352-3018(20)30359-3
The study describes the impact of the 2020 national COVID-19 lockdown on HIV testing and treatment in KwaZulu-Natal, South Africa, where 1,7 million people are living with HIV. While antiretroviral therapy (ART) provision was generally maintained, HIV testing and ART initiations were heavily impacted.
7 February
Abbott A. COVID’s mental-health toll: how scientists are tracking a surge in depression. Nature 2021, published 3 February. Full-text: https://www.nature.com/articles/d41586-021-00175-z
Researchers are using huge data sets to link changes in mental health to coronavirus response measures.
27 January
Leitner MC, Richlan F. Analysis System for Emotional Behavior in Football (ASEB-F): matches of FC Red Bull Salzburg without supporters during the COVID-19 pandemic. Humanit Soc Sci Commun 8, 14 (2021). Full-text: https://doi.org/10.1057/s41599-020-00699-1
Less aggression! This study (our “alternative” paper of the day) has evaluated the effect of missing crowds in football on the emotions and behavior of players, staff and officials. These data from Austria show that in “ghost games” overall, “emotional situations” declined by 20%. More data on this topic (other leagues, other sports) are eagerly awaited!
Chen CY, Chen IH, O’Brien KS et al. Psychological distress and internet-related behaviors between schoolchildren with and without overweight during the COVID-19 outbreak. Int J Obes (2021). Full-text: https://doi.org/10.1038/s41366-021-00741-5
Online survey among 1357 schoolchildren (mean age = 10,7 years), showing that overweight kids had significantly higher levels of COVID-19 infection fear, stress, depression, perceived weight stigma, and problematic social media use than those not overweight.
Partridge E, McCleery E, Cheema R, et al. Evaluation of Seasonal Respiratory Virus Activity Before and After the Statewide COVID-19 Shelter-in-Place Order in Northern California. JAMA Netw Open January 2021; 4(1):e2035281. Full-text: https://doi.org/10.1001/jamanetworkopen.2020.35281
Using interrupted time series analysis of testing for viral respiratory pathogens, this study found that statistically significant lower rates of common community respiratory viruses appeared to be associated with a shelter-in-place order during the coronavirus pandemic. Decreases were most pronounced for influenza (93%) and for rhinovirus or enterovirus (81%). Lower rates of post-exposure viral activity were seen for respiratory syncytial virus, parainfluenzavirus, coronaviruses, and adenoviruses, however, these associations were not statistically significant.
26 January
Verma AM, Patel A, Subramanian S, et al. From intravenous to subcutaneous infliximab in patients with inflammatory bowel disease: a pandemic-driven initiative. Lancet Gastroenterology Correspondence| Volume 6, ISSUE 2, P88-89, February 01, 2021. Full-text: https://doi.org/10.1016/S2468-1253(20)30392-7
Facing the clinical imperative to minimise patient exposure to hospital facilities to mitigate against the risk of nosocomial acquisition of COVID-19, the authors switched their patients with inflammatory bowel diseases (IBD) from intravenous to subcutaneous infliximab. Experiences are encouraging: in 31 IBD patients, this strategy appeared safe and enabled patients requiring infliximab to have home treatment self-administered at their convenience on the day of dose instead of having to attend a scheduled appointment at the hospital for an infusion.
23 January
Doubleday A, Choe Y, Busch Isaksen T, Miles S, Errett NA. How did outdoor biking and walking change during COVID-19?: A case study of three U.S. cities. PLoS One. 2021 Jan 20;16(1):e0245514. PubMed: https://pubmed.gov/33471858. Full-text: https://doi.org/10.1371/journal.pone.0245514
In Houston, bicycle use increased during lockdown. In New York, less people used their bikes. In Seattle, the results varied by trail use type. Read here why.
21 January
Li W, Zhang Y, Wang J, et al. Association of Home Quarantine and Mental Health Among Teenagers in Wuhan, China, During the COVID-19 Pandemic. JAMA Pediatr January 19, 2021. Full-text: https://doi.org/10.1001/jamapediatrics.2020.5499
During the COVID-19 quarantine period, more than 20% of adolescents had anxiety and depression. This is the result of an online questionnaire (using convenient sampling method) with 7890 teenagers from Wuhan. The prevalence was 21,7% (n = 1708) for anxiety and 24,6% (n = 1941) for depression (HADS subscale score > 7). Long-term home restrictions might have adverse effects on mental health of adolescents because of a sharp change of lifestyle and various other stressors like fear of infection, frustration, and boredom.
Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav (2021). Full-text: https://doi.org/10.1038/s41562-020-01042-z
In Japan, monthly suicide rates declined by 14% during the first 5 months of the pandemic (February to June 2020). This could be due to a number of complex reasons, including the government’s generous subsidies, reduced working hours and school closure. By contrast, monthly suicide rates increased by 16% during the second wave (July to October 2020), with a larger increase among females (37%) and children and adolescents (49%).
18 January
Wang J, Li Y, Musch DC, et al. Progression of Myopia in School-Aged Children After COVID-19 Home Confinement. JAMA Ophthalmol. 2021 Jan 14. PubMed: https://pubmed.gov/33443542. Full-text: https://doi.org/10.1001/jamaophthalmol.2020.6239
Home confinement during the COVID-19 pandemic may have been associated with a substantial myopic shift for younger school-aged children (6-8 years). In this cross-sectional study of 123.535 children, Xuehan Qian, Jiaxing Wang and colleagues found that the prevalence of myopia increased 1,4 to 3 times in 2020 compared with the previous 5 years. See also the comment by Klaver CCW, Polling JR, Enthoven CA. 2020 as the Year of Quarantine Myopia. JAMA Ophthalmol. 2021 Jan 14. PubMed: https://pubmed.gov/33443551. Full-text: https://doi.org/10.1001/jamaophthalmol.2020.6231
16 January
Morris JA, Goldacre R, Spata E, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol 2021, published 14 January. Full-text: https://doi.org/10.1016/S2468-1253(21)00005-4
Eva Morris et al.
Pandemic COVID-19 waves lead to a sustained reduction in the number of people referred, diagnosed, and treated for colorectal cancer. As compared to the monthly average in 2019, in April 2020 there was a 63% reduction (from 36.274 to 13.440) in the monthly number of 2-week referrals for suspected cancer and a 92% reduction in the number of colonoscopies (from 46.441 to 3484).
10 January
Adeniji N, Carr RM, Aby ES, Catana AM, Wegermann K, Dhanasekaran R. Socioeconomic Factors Contribute to the Higher Risk of COVID-19 in Racial and Ethnic Minorities with Chronic Liver Diseases (CLD). Gastroenterology. 2020 Nov 20:S0016-5085(20)35438-X. PubMed: https://pubmed.gov/33227281. Full-text: https://doi.org/10.1053/j.gastro.2020.11.035
Recent studies have shown that patients with chronic liver disease (CLD) in general, and especially those with decompensated cirrhosis and alcohol-related liver disease, are at higher risk COVID-19-related mortality. In this multi-center US cohort study, Renumathy Dhanasekaran, Nia Adeniji and colleagues included 909 patients with CLD and COVID-19 from 21 US centers. They show that non-Hispanic Blacks (NHB) and Hispanics are disproportionately represented in patients with CLD who acquire COVID-19. Both non-Hispanic Blacks and Hispanics had lower household income, lower rates of private insurance, and Hispanics had higher rates of being uninsured. Additionally, the authors show that both NHB and Hispanics had a higher likelihood of living in multifamily housing and in neighborhoods with higher rates of poverty and overcrowding than non-Hispanic Whites.
8 January
Sarvey D, Welsh JW. Adolescent substance use: Challenges and opportunities related to COVID-19. J Subst Abuse Treat. 2020 Nov 24:108212. PubMed: https://pubmed.gov/33272731. Full-text: https://doi.org/10.1016/j.jsat.2020.108212
Adolescent substance use is a significant and largely undertreated public health concern. The COVID-19 pandemic has exacerbated many pre-existing risk factors for adolescent substance use, such as early life stress, social isolation, school connections, and boredom. Here, Dana Sarvey and Justine Welsh give a short overview of changing risk and protective factors for substance use and potential opportunities during the pandemic. They recommend that practitioners should consider any and all means of reaching out to these youth and their families and addressing other co-occurring psychiatric symptoms, such as depression and anxiety.
7 January
Evans DP, Hawk SR, Ripkey CE. Domestic Violence in Atlanta, Georgia Before and During COVID-19. Violence Gend 2020, published 11 December. Full-text: https://doi.org/10.1089/vio.2020.0061
Cumulative counts of domestic crimes were higher during the COVID-19 period of 2020 than in the preceeding two years suggesting increased occurrence of domestic violence, especially during shelter-in-place orders. This is the result of an analysis of 30 weeks of crime data collected from the Atlanta Police Department (APD). Dabney Evans, Shila René Hawk and Carrie Ripkey found that a spike in domestic crimes was recorded after city and statewide shelter-in-place orders. The authors summarize that the “co-occurring pandemics of COVID-19 and domestic violence come amidst a period of racial justice reckoning in the United States and that both have a disproportionate impact on Black, Indigenous, and People of Color. As the country grapples with how to deal with health and safety concerns related to the pandemic, and the unacceptable harms being perpetrated by police, a public health approach is strongly warranted to address both universal health care and violence prevention.”
5 January
COVIDSurg Collaborative. Head and neck cancer surgery during the COVID-19 pandemic: An international, multicenter, observational cohort study. Cancer. 2020 Dec 21. PubMed: https://pubmed.gov/33345297. Full-text: https://doi.org/10.1002/cncr.33320
Head and neck cancer surgery in the COVID‐19 era appears safe even when surgery is prolonged and complex. This is the result of an international, observational cohort study comprised of 1137 consecutive patients with head and neck cancer undergoing primary surgery with curative intent in 26 countries. The overall 30‐day mortality was 1.2%. Twenty‐nine patients (3%) tested positive for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) within 30 days of surgery; 13 of these patients (44.8%) developed severe respiratory complications, and 3 (10.3%) died. There were significant correlations with an advanced tumor stage and admission to critical care.
Note of the editor: The original text said: “and 3.51 (10.3%) died.” Too much alcohol during pre-Christmas proof-reading?
Seitlinger J, Wollbrett C, Mazzella A, et al. Safety and feasibility of thoracic malignancy surgery during the COVID-19 pandemic. Ann Thorac Surg. 2020 Dec 14:S0003-4975(20)32115-9. PubMed: https://pubmed.gov/33333085. Full-text: https://doi.org/10.1016/j.athoracsur.2020.12.001
Maintaining surgical oncologic activity in the era of the COVID-19 pandemic seems safe and feasible, with low postoperative morbidity and mortality. The authors collected data on thoracic malignancy surgeries from January 1 to April 30, 2020, including patients from high-volume thoracic surgery departments in Nancy, Strasbourg, Freiburg, Milano, Torino and Montreal. In the cohort of 731 patients, 9 cases (1.2%) of COVID-19 were confirmed by PCR, including 5 in-hospital contaminants. The total number of deaths was 22 (3%). Only one death was related to COVID-19 (0,14%).
4 January
Kosten TR, Petrakis IL. The Hidden Epidemic of Opioid Overdoses During the Coronavirus Disease 2019 Pandemic. JAMA Psychiatry. 2020 Dec 30. PubMed: https://pubmed.gov/33377967. Full-text: https://doi.org/10.1001/jamapsychiatry.2020.4148
An unexpected tragedy of the coronavirus disease 2019 (COVID-19) pandemic is increased opioid and fentanyl overdoses, since many factors could have helped in reducing opioid use disorder (OUD) and overdoses during the pandemic. Follow Thomas Kosten and Ismene Petrakis on this short trip through drug addiction and society’s response.
2 January
Van Haren RM, Delman AM, Turner KM, et al. Impact of the COVID-19 Pandemic on Lung Cancer Screening Program and Subsequent Lung Cancer. J Am Coll Surg. 2020 Dec 12:S1072-7515(20)32525-4. PubMed: https://pubmed.gov/33346080. Full-text: https://doi.org/10.1016/j.jamcollsurg.2020.12.002
Low-dose computed tomography (LDCT) screening reduces lung cancer mortality by at least 20%. At the University of Cincinnati, COVID-19 caused significant disruption in lung cancer screening, leading to a decrease in new patients screened and an increased proportion of nodules suspicious for malignancy once screening resumed.
1 January
Rattka M, Dreyhaupt J, Winsauer C, et al. Effect of the COVID-19 pandemic on mortality of patients with STEMI: a systematic review and meta-analysis. Heart. 2020 Dec 17:heartjnl-2020-318360. PubMed: https://pubmed.gov/33334863. Full-text: https://doi.org/10.1136/heartjnl-2020-318360
In this meta-analysis, the authors assessed outcomes of 50.123 patients from 10 studies. Did the analyzed data show that acute and timely medical care of these patients had been maintained during the pandemic in most countries? Yes, they did. Consequently, despite a significant reduction in overall admission rates of patients with STEMI during the COVID-19 pandemic (incidence rate ratio = 0.789, 95% CI 0.730 to 0.852, I2=77%, p < 0.01), there was no significant difference in hospital mortality (OR = 1.178, 95% CI 0.926 to 1.498, I2=57%, p = 0.01) compared with patients with STEMI admitted before the outbreak.
31 December
Santoro GA, Grossi U, Murad-Regadas S, et al. DElayed COloRectal cancer care during COVID-19 Pandemic (DECOR-19): Global perspective from an international survey. Surgery. 2020 Nov 17:S0039-6060(20)30778-9. PubMed: https://pubmed.gov/33353731. Full-text: https://doi.org/10.1016/j.surg.2020.11.008
The authors analyzed the impact of the SARS-CoV-2 pandemic on pre-operative assessment, elective surgery, and post-operative management of colorectal cancer patients, using a 35-item survey, which was answered by a total of 1051 respondents from 84 countries. The result: both diagnostic and therapeutic practices changed. Endoscopic and radiologic procedures were highly affected and elective CRC surgery was impacted for almost all respondents (97,3%), with planned procedures being temporarily suspended (46,8%) or capacity reduced (50,5%).
30 December
Mourouvaye M, Bottemanne H, Bonny G, et al. Association between suicide behaviours in children and adolescents and the COVID-19 lockdown in Paris, France: a retrospective observational study. Arch Dis Child. 2020 Dec 22:archdischild-2020-320628. PubMed: https://pubmed.gov/33355154. Full-text: https://doi.org/10.1136/archdischild-2020-320628
There was a 50% decrease in the incidence of suicidal behaviors in children and adolescents during the COVID-19 lockdown in Paris, France. The authors of this retrospective observational study conducted in Necker Hospital for Sick Children, Paris (January 2018–June 2020), speculate about the reasons for this decline.
29 December
Gergen AK, Madsen HJ, Tilva KR, Smith JB, Weyant MJ. Coronavirus Disease 2019 in Lung Transplant Recipients. Ann Thorac Surg. 2020 Dec 18:S0003-4975(20)32134-2. PubMed: https://pubmed.gov/33347850. Full-text: https://doi.org/10.1016/j.athoracsur.2020.11.032
The authors report risk factors, clinical manifestations, and treatment course of two lung transplant recipients diagnosed with COVID-19 pneumonia. After being hospitalized and later discharged home, both patients were readmitted several days later with significant worsening of respiratory status and infectious symptoms.
Martire LM, Isaacowitz DM. What Can We Learn About Psychological Aging By Studying Covid-19? The Journals of Gerontology: Series B 2020, published 26 December. Full-text: https://doi.org/10.1093/geronb/gbaa217
The authors give a short overview of papers about Americans living under varying social and travel restrictions; individuals living in Sweden during a period of voluntary social distancing; individuals living in Spain during a mandatory lockdown; older age predicting better or worse functioning; the ability of elderly people to deal with adversity; and the importance of using behavioral research to reduce ageism and promote intergenerational solidarity.
26 December
Silverman ME, Burgos L, Rodriguez ZI, et al. Postpartum mood among universally screened high and low socioeconomic status patients during COVID-19 social restrictions in New York City. Sci Rep 10, 22380 (2020). Full-text: https://doi.org/10.1038/s41598-020-79564-9
Post-partum depression, the most common complication of childbearing, is a prevalent, cross-cultural disorder. Even in the best environments, the period following childbirth represents a time of heightened stress and vulnerability for most, if not all, new parents. In this study of 516 post-partum patients, Michael Silverman et al. now demonstrate a differentiated response in the post-partum mood of those living in New York City during the COVID-19 pandemic… based on socioeconomic status! While those in areas with higher socioeconomic status (SES) demonstrated no change in post-partum mood after implementation of social restrictions in New York, those living in lower SES expressed improved mood over the same time period. Try to find out why.
16 December
Jones N. How COVID-19 is changing the cold and flu season. Nature 2020, published 15 December. Full-text: https://www.nature.com/articles/d41586-020-03519-3
By mid-December, the Northern Hemisphere is usually well into the start of its annual cold and flu season — but so far this year, even as the COVID-19 pandemic surges in dozens of countries, the levels of many common seasonal infections remain extremely low. Measures meant to tame the coronavirus pandemic are quashing influenza and most other respiratory diseases, which could have wide-ranging implications.
15 December
Ma X, Guan C, Chen R, et al. Pathological and molecular examinations of postmortem testis biopsies reveal SARS-CoV-2 infection in the testis and spermatogenesis damage in COVID-19 patients. Cell Mol Immunol (2020). Full-text: https://doi.org/10.1038/s41423-020-00604-5
Yesterday, we reported about sexual desire, weekly sexual intercourse/masturbation number, foreplay time, and sexual intercourse which might be somewhat decreased in COVID times (see https://covidreference.com/top-10-december-14). Now Shuiqiao Yuan, Xixiang Ma and colleagues from Huazhong University of Science and Technology, Wuhan, evaluated the effects of SARS-CoV-2 infection on spermatogenesis by examining the pathophysiology and molecular features of testes obtained from five male COVID-19 patients at autopsy. Their findings might provide evidence that SARS-CoV-2 can infect the testis and germ cells, indicating the potential impact of the COVID-19 pandemic on spermatogenesis and male fertility.
12 December
Kapur N, Clements C, Appleby L, et al. Impact of the Covid-19 pandemic on the frequency of primary care-recorded mental illness and self-harm episodes in the UK: population-based cohort study of 14 million individuals. Lancet Psychiatry 2020, published 10 December. Full-text: https://doi.org/10.1016/S2215-0366(20)30528-9
Self-harm often precedes suicide and can be used as a proxy outcome to identify how the pandemic has affected population mental health. As yet, there is no indication that the pandemic has caused self-harm rates to increase in the UK. The authors cite a study of 1500 general practices in the UK which found that the recorded incidence of self-harm was 38% lower in April, 2020, than the rate expected on the basis of previous years (Carr MJ, Steeg S, Webb RT, et al). Primary care contact for mental illness and self-harm before, during and after the peak of the COVID-19 pandemic in the UK: cohort study of 13 million individuals. Lancet Public Health (in press)). This decrease was particularly marked in women, people younger than 45 years, and those from the most deprived quintile of practices.
11 December
Mackie SL, Brouwer E, Conway R, et al. Clinical pathways for patients with giant cell arteritis during the COVID-19 pandemic: an international perspective. Lancet Rheumatol 2020, published 8 December. Full-text: ???
Giant cell arteritis, a common primary systemic vasculitis affecting older people, presents acutely as a medical emergency and requires rapid specialist assessment and treatment to prevent irreversible vision loss. The authors show that during the COVID-19 pandemic, patients might be involved in the reshaping of clinical services.
10 December
Pun KY, Kok AA, Eikelenboom M. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry December 08, 2020. Full-text: https://doi.org/10.1016/S2215-0366(20)30491-0
Between April 1 and May 13, 2020, online questionnaires were distributed among ongoing cohorts from the Netherlands, including people with (n = 1181) and without (n = 336) depressive, anxiety, or obsessive-compulsive disorders. People without depressive, anxiety, or obsessive-compulsive disorders showed a greater increase in symptoms during the COVID-19 pandemic, whereas individuals with the greatest burden on their mental health tended to show a slight symptom decrease.
8 December
Friedman J, Beletsky L, Schriger DL. Overdose-Related Cardiac Arrests Observed by Emergency Medical Services During the US COVID-19 Epidemic. JAMA Psychiatry December 3, 2020. 2020. Full-text: https://doi.org/10.1001/jamapsychiatry.2020.4218
The authors leveraged a large, national US EMS database to characterize emergent trends in overdose mortality fueled by the pandemic. They describe a large-magnitude, national surge in overdose-related cardiac arrest during the initial months of the COVID-19 epidemic in the US. Peak rates in May 2020 were more than double the baseline from 2018 and 2019, and overall 2020 values were elevated by approximately 50%. Results suggest that the fallout from the COVID-19 pandemic—perhaps especially social isolation—is sharply accelerating fatal overdose trends.
7 December
Heaton HA, Luke A, Sztajnkrycer MD, Clements CM, De Moraes AG, Raukar NP. Best Practices in Managing Cardiac Arrest in the Emergency Department During the COVID-19 Pandemic. Mayo Clin Proc. 2020 Dec;95(12):2704-2708. PubMed: https://pubmed.gov/33276842. Full-text: https://doi.org/10.1016/j.mayocp.2020.10.009
Patients with COVID-19 are at increased risk of cardiac complications including cardiac arrest. Of admitted patients, almost 30% may have evidence of myocardial injury with mortality among hospitalized patients as high as 70%. The resuscitation of these patients requires a conscious effort to minimize the spread of SARS-CoV-2. The authors present a best-practice model based on four guiding principles: (1) reduce the risk of exposure to the entire health care team; (2) decrease the number of aerosol-generating procedures; (3) use a small resuscitation team to limit potential exposure; and (4) consider early termination of resuscitative efforts.
Fuady A, Houweling TAJ, Richardus JH. COVID-19 and Tuberculosis-Related Catastrophic Costs. Am J Trop Med Hyg. 2020 Dec 2. PubMed: https://pubmed.gov/33269683. Full-text: https://doi.org/10.4269/ajtmh.20-1125
Interruptions of TB control programs could potentially prolong diagnostic delays and worsen TB treatment outcomes. In addition, the upcoming economic recession could lead to a reduction of income and a rise in unemployment rates in TB-affected households. All of these factors increase the risk of TB incidence and the economic impact on TB-affected households.
Indini A, Cattaneo M, Ghidini M, et al. Triage process for the assessment of coronavirus disease 2019-positive patients with cancer: The ONCOVID prospective study. Cancer. 2020 Dec 3. PubMed: https://pubmed.gov/33270908. Full-text: https://doi.org/10.1002/cncr.33366
General measures to keep COVID‐19–free cancer divisions have been adopted worldwide. In this prospective clinical trial, the authors evaluated the efficacy of triage to identify COVID‐19 among patients with cancer. Of 562 enrolled patients, 6 (1%) were diagnosed with COVID‐19, of whom 4 (67%) had the disease detected through telehealth triage, and 2 patients (33%) without suspect symptoms at triage had the disease detected later. The authors conclude that telehealth triage was helpful in detecting suspect patients and to keep a COVID‐19–free cancer center. The overall incidence of COVID‐19 diagnosis (1%) and antibody positivity (13%) in patients with suspect symptoms was similar to that observed in the general population.
Peach E, Rutter M, Lanyon P, et al. Risk of death among people with rare autoimmune diseases compared to the general population in England during the 2020 COVID-19 pandemic. Rheumatology (Oxford). 2020 Dec 4:keaa855. PubMed: https://pubmed.gov/33271595. Full-text: https://doi.org/10.1093/rheumatology/keaa855
The risk of all-cause death is more prominently heightened during COVID-19 among people with rare autoimmune rheumatic diseases (RAIRD) than among the general population. This is a result of an analysis which included 168.691 people with a recorded RAIRD diagnosis alive on 01/03/2020. The age-standardized mortality rate (ASMR) among people with RAIRD was 1.44 times higher than the average ASMR during the same months of the previous 5 years, whereas in the general population of England it was 1.38 times higher. The authors suggest quantifying how much risk is due to COVID-19 and how much is due to a disruption to healthcare services.
2 Dezember
Perez S, Innes GK, Walters MS, et al. Increase in Hospital-Acquired Carbapenem-Resistant Acinetobacter baumannii Infection and Colonization in an Acute Care Hospital During a Surge in COVID-19 Admissions — New Jersey, February–July 2020. MMWR Morb Mortal Wkly Rep. ePub: 1 December 2020. Full-text: http://dx.doi.org/10.15585/mmwr.mm6948e1
Carbapenem-resistant Acinetobacter baumannii (CRAB) causes health care–associated infections that are challenging to contain and often linked to infection prevention and control breaches. What a mess: colleagues from a New Jersey hospital report on a cluster of 34 CRAB cases (26 isolates harbored the gene encoding the OXA-23 carbapenemase) that peaked during a surge in COVID-19 hospitalizations. The authors conclude that strategies to preserve continuity of care led to deviations in IPC practices; CRAB cases decreased when normal operations resumed.
Armitaage R, Nellums B. Antibiotic prescribing in general practice during COVID-19. Lancet December 01, 2020. Full-text: https://doi.org/10.1016/S1473-3099(20)30917-8
Richard Armitage and Laura B Nellums comment on the number of antibiotic prescriptions made in UK general practice between April 1, and Aug 31, 2020. The number was 15% lower than in the corresponding period in 2019. However, given the decrease in absolute number of appointments over this time, this number of prescriptions was 7% higher than expected, supporting evidence that antibiotic prescribing rates are higher in remote consultations than during in-person appointments.
30 November
Singhai R, Tahrani AA, Ludwig C, et al. Global 30-day outcomes after bariatric surgery during the COVID-19 pandemic (GENEVA): an international cohort study. Lancet Diabetes Endocrinology November 27, 2020. Full-text: https://doi.org/10.1016/S2213-8587(20)30375-2
This international cohort study GENEVA investigated the outcomes of bariatric and metabolic surgery (BMS) performed in 2116 adults (≥ 18 years) between May 1 and July 10 from 133 hospitals in 38 countries. Overall, 30-day morbidity and mortality following BMS during the COVID-19 pandemic with locally appropriate perioperative COVID-19 protocols in place seemed to be similar to pre-pandemic levels. Of the ten patients with symptomatic post-operative COVID-19, none needed ventilation and none died.
29 November
Simões D, Stengaard AR, Combs L, The EuroTEST COVID-19 impact assessment consortium of partners. Impact of the COVID-19 pandemic on testing services for HIV, viral hepatitis and sexually transmitted infections in the WHO European Region, March to August 2020. Euro Surveill 2020;25(47):pii=2001943. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.47.2001943
The pandemic has had considerable impact on testing for HIV, viral hepatitis and STIs in the WHO European Region. Preliminary results show that 95% of respondents from 34 countries reported testing less than half the expected number of people during the first months of the COVID-19 pandemic between March and May 2020. This continued, although to a lesser degree, between June and August 2020, when measures were less strict in most countries.
Sullivan SG, Carlson S, Cheng AC, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill. 2020;25(47). Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.47.2001847
In Australia, influenza activity was at an all-time low during the southern hemisphere’s 2020 winter. The 2020 pandemic restrictions may substantially ameliorate winter respiratory pathogen epidemics in 2021 and beyond.
28 November
Clark JJ, Dwyer D, Pinwill N, Clark P, Johnson P, Hackshaw A. The effect of clinical decision making for initiation of systemic anticancer treatments in response to the COVID-19 pandemic in England: a retrospective analysis. Lancet Oncol 2020, published 27 November. Full-text: https://doi.org/10.1016/S1470-2045(20)30619-7
During the 2020 spring lockdown and immediately thereafter, there was an important reduction in systemic anti-cancer treatment initiation in England: 32% in April and 10% in May. In June, the number of registrations for new systemic anti-cancer treatments increased by 15% compared to the 6 pre-COVID months (September, 2019, to February, 2020). James Clark et al. recommend continuing to assess the effects of delaying treatment initiation for advanced cancers and neoadjuvant therapies.
24 November
Morgan L, Protopopova A, Birkler RID, et al. Human–dog relationships during the COVID-19 pandemic: booming dog adoption during social isolation. Humanit Soc Sci Commun 7, 155 (2020). Full-text: https://doi.org/10.1057/s41599-020-00649-x
Good news (for dogs) from Israel: the stricter the social isolation became during the COVID-19 pandemic, the greater the interest in dog adoption. Dog abandonment has decreased and the rates of dog adoptions improved significantly; the demand for adoptable dogs and the requests to serve as foster families increased significantly, and accordingly, the length of stay of dogs at the shelter was significantly shorter.
18 November
De Luca G, Verdoia M, Cercek M, et al. Impact of COVID-19 Pandemic on Mechanical Reperfusion for Patients With STEMI. J Am Coll Cardiol. 2020 Nov 17;76(20):2321-2330. PubMed: https://pubmed.gov/33183506. Full-text: https://doi.org/10.1016/j.jacc.2020.09.546
A total of 6609 patients underwent primary percutaneous coronary intervention (PPCI) in 77 centers, located in 18 countries. In 2020, during the pandemic, there was a significant reduction in PPCI as compared with 2019 (incidence rate ratio: 0.81; 95% confidence interval: 0.78 to 0.84). Furthermore, the pandemic was associated with a significant increase in “door-to-balloon” and total ischemia times, which may have contributed to higher mortality during the pandemic.
17 November
Leske S, Kõlves K, Cromton D, et al. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry, November 16, 2020. Full-text: https://doi.org/10.1016/S2215-0366(20)30435-1
Do suicide rates increase during infectious disease outbreaks? Probably not (at least in Australia). In this study, analyzing suspected suicide rates in 2020 relative to 2015–19 to assess any early effects of the COVID-19 pandemic in Queensland, no evidence of a change in suspected suicide rates was seen.
15 November
Monnet DL, Harbarth S. Will coronavirus disease (COVID-19) have an impact on antimicrobial resistance? Euro Surveill. 2020;25(45):pii=2001886. Full-text: https://doi.org/10.2807/1560-7917.ES.2020.25.45.2001886.
Good question. We don’t know yet. After summarizing various determinants that may result in either an increase or, inversely, a decrease in antimicrobial resistance (AMR), the authors found them to be balanced. The truth is that the impact of the COVID-19 pandemic on AMR will only become clear in the coming months and years as data gradually become available. Changes in AMR will most likely vary depending on the setting—e.g., ICUs vs other hospital units, hospital vs community settings—and possibly between countries.
Chan PS, Girotra S, Tang Y. Outcomes for Out-of-Hospital Cardiac Arrest in the United States During the Coronavirus Disease 2019 Pandemic. JAMA Cardiology November 14, 2020, Full-text: https://doi.org/10.1001/jamacardio.2020.6210
What is the association between the SARS-CoV-2 pandemic and out-of-hospital cardiac arrest (OHCA) outcomes in the US? This large registry study of 19,303 cases in 2019 and 2020 showed that the return of spontaneous circulation (ROSC) for OHCA was 18% lower overall than before the pandemic. Although the decrease was more prominent in counties most affected by the COVID-19 pandemic, lower rates of sustained ROSC and higher rates of termination of resuscitation were also observed in counties with low COVID-19 mortality rates. Delays in seeking medical care during the lockdown may not entirely explain the findings. The authors speculate that the interim recommendations for emergency medical service during this pandemic (for protecting frontline health care workers from unnecessary exposure) may also have decreased the likelihood of a successful resuscitation.
11 November
Abdallah HO, Zhao C, Kaufman E, et al. Increased Firearm Injury During the COVID-19 Pandemic: A Hidden Urban Burden. J Am Coll Surg. 2020 Oct 26:S1072-7515(20)32413-3. PubMed: https://pubmed.gov/33166665. Full-text: https://doi.org/10.1016/j.ja mcollsurg.2020.09.028
Lockdown causes domicile discord which in turn causes more penetrating trauma? Jose Pascual, Hatem Abdallah and colleagues tested the hypothesis that intentional injury might have increased during stay-at-home-orders (SAHO) and assessed injury patterns from 6 weeks pre- to 10 weeks post- statewide stay-at-home order. 357 and 480 trauma patients presented pre- and post-SAHO, respectively. Pre- and post- groups demonstrated differences in sex, age, and race. Post-SAHO mechanism of injury (blunt vs. penetrating) revealed more intentional injury.
Lee PH, Marek J, Nálevka P. Sleep pattern(s) in the US and 16 European countries during the COVID-19 outbreak using crowdsourced smartphone data. Eur J Public Health 2020, published 10 November. Full-text: https://doi.org/10.1093/eurpub/ckaa208
When you sleep, your smartphone is taking notes and you may end up in a scientific publication. Here Paul Lee and colleagues utilized a large crowdsourced database (Sleep as Android) and analyzed the (your?) sleep behavior of 25,217 users with 1,352,513 sleep records between 1st January and 29th April 2020 in 16 European countries (Germany, United Kingdom, Spain, France, Italy, the Netherlands, Belgium, Hungary, Denmark, Finland, Norway, Czech, Sweden, Austria, Poland, and Switzerland) and in the US. The unsurprising result: during lockdown, people delayed their bedtime and slept longer than usual.
9 November
Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2020 Oct 27. PubMed: https://pubmed.gov/33108269. Full-text: https://doi.org/10.5664/jcsm.8930
Forty-four papers, involving a total of 54,231 participants from 13 countries, contributed to this systematic review and meta-analysis of sleep problems during COVID-19. The global pooled prevalence rate of sleep problems among all populations was 35,7%. COVID-19 patients appeared to be the most affected group, with a pooled rate of 74,8%. Healthcare workers and the general population had comparative rates of sleep problems with rates of 36,0% and 32,3%, respectively.
Dyer O. Covid-19: Denmark to kill 17 million minks over mutation that could undermine vaccine effort. BMJ 2020; 371:m4338. Full-text: https://doi.org/10.1136/bmj.m4338
Among 5102 samples of virus taken from Danish patients since June, five infection clusters affecting 214 people involved mink variant virus. One of these, known as cluster 5, seems to be a problematic variant which could be less susceptible to some antibodies and/or vaccines (unproven). This variant has been detected with four simultaneous changes in the genes for the Spike protein (for nerds: H69del/V70del, Y453F, I692V and M1229I) and has affected 11 people in North Jutland. Conclusion: 17 million minks will be culled.
5 November
Huh K, Jung J, Hong J, et al. Impact of non-pharmaceutical interventions on the incidence of respiratory infections during the COVID-19 outbreak in Korea: a nationwide surveillance study. Clin Infect Dis 2020, published 5 November. Full-text: https://doi.org/10.1093/cid/ciaa1682
Non-pharmaceutical interventions (NPIs) implemented to slow the spread of SARS-CoV-2 have led to the decline in the incidences of highly transmissible respiratory infections. This is the result of a study by Ji-Man Kang, Kyungmin Huh and colleagues from the Children’s Hospital, Yonsei University College of Medicine, Seoul. Comparing the period February–July 2020 to the previous 4 years, the authors found that the incidences of chickenpox and mumps were significantly lower than in the prediction model (chickenpox: 36%, mumps: 63%).
2 November
Qu Z, Oedingen C, Bartling T, Schrem H, Krauth C. Organ procurement and transplantation in Germany during the COVID-19 pandemic. Lancet. 2020 Oct 31;396(10260):1395. PubMed: https://pubmed.gov/33129390. Full-text: https://doi.org/10.1016/S0140-6736(20)32213-3
No damage in this area: Compared with the previous year, the cumulative numbers of deceased organ donors and transplants showed no significant reduction in Germany. Kidney transplantation numbers were stable, while the numbers of heart, lung, and liver transplantations from deceased donors even increased from January to April, 2020, when compared with the same period of the previous year. In contrast, transplant activities in Italy and Spain were reduced by 30–50%.
Sors F, Grassi M, Agostini T, Murgia M. The sound of silence in association football: Home advantage and referee bias decrease in matches played without spectators. Eur J Sport Sci. 2020 Nov 1;1-21. Full-text: https://doi.org/10.1080/17461391.2020.1845814
We have eagerly awaited this news for decades: spectators can significantly contribute to determine the dynamics and the outcomes of professional football matches (home advantage and referee bias are two well-documented phenomena in professional sports). COVID-19 has made it possible: focusing on the first and second divisions of the top four UEFA countries, the authors analyzed 841 matches behind closed doors during the pandemic. This extremely important work revealed that observed frequencies for home victories, draws and away victories were significantly different from the expected frequencies calculated based on the last three complete seasons with spectators. The absence of a referee bias in favor of the home teams for yellow cards indicated that this factor might be particularly affected by the presence/absence of social pressure by spectators. Various parameters were considered, and the analyses revealed a reduction of home advantage and the absence of referee bias. They´ll walk alone now.
30 October
Garrett-Mayer E, Rini BI. To Treat or Not to Treat—Balancing Benefits and Risks of Treatment Delay Among Patients With Cancer During the COVID-19 Pandemic. JAMA Oncol 2020, published 29 October. Full-text: https://doi.org/10.1001/jamaoncol.2020.4886
To treat or not to treat after balancing the benefits and risks of immediate treatment for cancer with the potential risk of COVID-19 and its associated complications, including death? Elizabeth Garrett-Mayer and Brian Rini discuss the paper by Hartman HE, Sun Y, Devasia TP, et al: Integrated Survival Estimates for Cancer Treatment Delay Among Adults With Cancer During the COVID-19 Pandemic. JAMA Oncol 2020, published 29 October. Full-text: https://doi.org/10.1001/jamaoncol.2020.5403
25 October
Wathelet M, Duhem S, Vaiva G, et al. Factors Associated With Mental Health Disorders Among University Students in France Confined During the COVID-19 Pandemic. JAMA Netw Open October 23, 2020. 2020;3(10):e2025591. Full-text: https://doi.org/10.1001/jamanetworkopen.2020.25591
This nation-wide survey study of 69,054 students from France who experienced quarantine found high prevalence rates of severe self-reported mental health symptoms, including suicidal thoughts (11%), severe distress (22%), high level of perceived stress (25%), severe depression (16%), and high level of anxiety (28%). Among risk factors identified, female or nonbinary gender, problems with income or housing, history of psychiatric follow-up, symptoms compatible with COVID-19, social isolation, and low quality of information received were associated with altered mental health. Main limitation is that the population represented only 4.3% of students contacted and that self-selection bias may have altered the results. However, they are suffering.
21 October
Mohamed MO, Banerjee A, Clarke S, et al. Impact of COVID-19 on cardiac procedure activity in England and associated 30-day mortality. Eur Heart J 2020, published 20 October. Full-text: https://doi.org/10.1093/ehjqcco/qcaa079
A preview of what cardiology departments might see in the coming autumn and winter months 2020/2021. The authors analyzed the impact of COVID-19 on changes in cardiac procedure activity in England. Compared to the monthly averages (March-May) in 2018/2019, there was a deficit of 45,501 procedures between 1st January and 31st May 2020. Cardiac catheterization and device implantations were the most affected in terms of numbers (n = 19,637 and n = 10,453). No difference in 30-day mortality was observed between pre-COVID and COVID time-periods for all cardiac procedures except cardiac catheterization and cardiac device implantation.
18 October
Marchetti D, Fontanesi L, Mazza C, et al. Parenting-Related Exhaustion During the Italian COVID-19 Lockdown. Journal of Pediatric Psychology,17 October 2020. Full-text: https://doi.org/10.1093/jpepsy/jsaa093
Who suffers the most? While many countries prepare for a second lockdown, this study took a look on the psychological consequences during the first wave, performing interviews with a total of 1226 parents via a demographic questionnaire. Seventeen percent reported significant parenting-related exhaustion and most parents reported a clinically alarming level of distress. Multiple regression analyses showed that greater parenting-related exhaustion was predicted by psychological distress, lower parental resilience, motherhood, fewer perceived social connections, and being single, as well as having a child with special needs, having a large number of children, and having younger children.
14 October
Been JV, Burgos Ochoa L, Bertens LCM. Impact of COVID-19 mitigation measures on the incidence of preterm birth: a national quasi-experimental study. Lancet Public Health 2020, published 13 October. Full-text: https://doi.org/10.1016/S2468-2667(20)30223-1
In this large national quasi-experimental study spanning a 10-year period, substantial reductions in preterm births were observed following implementation of the first national COVID-19 mitigation measures in the Netherlands on March 9, 2020. Babies born at the lowest gestational ages and those with the lowest birthweights were consistently underrepresented in our cohort throughout the study period.
3 October
Bakouny Z, Hawley JE, Choueiri TK, et al. COVID-19 and Cancer:Current Challenges and Perspectives. Cancer Cell 2020, published 1 October. Full-text: https://doi.org/10.1016/j.ccell.2020.09.018
The SARS-CoV-2 pandemic has affected patients with cancer in many ways (adverse outcomes in those who developed COVID-19, impact on the delivery of cancer care, etc.). In this review, the authors discuss the biological interplay between the two diseases and give practical recommendations for the management of patients with cancer during the pandemic. They also provide some insights from the cancer research community that might help develop novel therapies for all patients with COVID-19.
27 September
Weiss DJ, Bertozzi-Villa A, Rumisha SF, et al. Indirect effects of the COVID-19 pandemic on malaria intervention coverage, morbidity, and mortality in Africa: a geospatial modelling analysis. Lancet Infect Dis 2020, published 25 September. Full-text: https://doi.org/10.1016/S1473-3099(20)30700-3
Under pessimistic scenarios, COVID-19-related disruption to malaria control in Africa could almost double malaria mortality in 2020, and potentially lead to even greater increases in subsequent years.
Ueda Oshima M, Sandmaier BM, Petersdorf E, et al. Blood and marrow transplantation during the emerging COVID-19 pandemic: the Seattle approach. Bone Marrow Transplant 2020, published 26 September. Full-text: https://doi.org/10.1038/s41409-020-01068-x
Increasing numbers of COVID-19 hospitalizations and deaths, pandemic-related stresses on healthcare resources, shelter-in-place public health measures – how can you safely perform potentially life-saving stem cell transplants in this setting? Masumi Oshima et al. describe the challenges and the collateral impact of directing clinical resources toward COVID-19-related care on cancer patients in need of stem cell transplantation.
17 September
Evans ML, Lindauer M, Farrell ME. A Pandemic within a Pandemic — Intimate Partner Violence during Covid-19. N Engl J Med 2020, published 16 September. Full-text: https://doi.org/10.1056/NEJMp2024046
Stay-at-home orders led to many workers being furloughed, laid off, or told to work from home. They also left many intimate partner violence victims trapped with their abusers. Megan Evans, Margo Lindauer and Maureen Farrell put the 2020 lockdown experiences into perspective.
27 August
Hamadani JD, Hasan MI, Baldi AJ, et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Global Health 2020, published 25 August. Full-text:: https://doi.org/10.1016/S2214-109X(20)30366-1
In many countries, lockdowns exacerbate the risk of food insecurity and intimate partner violence. Here Sant-Rayn Pasricha, Jena Derakhshani Hamadani and colleagues analyze the impact lockdown orders on women and their families in rural Bangladesh. They randomly selected and invited the mothers of 3016 children to participate in the study, 2424 of whom provided consent. Almost all women reported a reduction in paid work for the family. Median monthly family income fell from US$212 at baseline to $59 during lockdown, and the proportion of families earning less than $1·90 per day rose from almost 0% to 47%. Before the pandemic, 5.6% and 2.7% experienced moderate and severe food insecurity, respectively. This increased to 36.5% and 15.3% during the lockdown. Find more information about intimate violence (emotional, physical, sexual).
25 August
Lee LYW, Cazier JB, Starkey T, et al. COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol 2020, published 24 August. Full-text: https://doi.org/10.1016/S1470-2045(20)30442-3
Patients with cancer have been reported to be at increased risk of infection with SARS-CoV-2 and a more severe disease course. Here Gary Middleton, Lennard Lee and colleagues compare cancer patients with and without COVID-19 and analyses the effect of tumor features (primary subtype and stage) and patient demographics (age and sex) on the risk and trajectory of COVID-19 disease. Some results:
- The all-cause case–fatality rate in patients with cancer after SARS-CoV-2 infection was significantly associated with increasing age, rising from 0.10 in patients aged 40–49 years to 0.48 in those aged 80 years and older.
- Patients with hematological malignancies (leukemia, lymphoma, and myeloma) had a more severe COVID-19 trajectory compared with patients with solid organ tumors.
- Patients with hematological malignancies who had recent chemotherapy had an increased risk of death during COVID-19-associated hospital admission (odds ratio 2.09).
Malik AA, Safdar N, Chandir S, et al. Tuberculosis control and care in the era of COVID-19. Health Policy and Planning 2020, published 24 August. Full-text: https://doi.org/10.1093/heapol/czaa109
Reports from India, China and Pakistan suggest a daily decline in tuberculosis case notification of 75 – 80% in the last few months with testing in Pakistan decreasing up to 80%. Is this the end of the Zero TB Initiative launched in October 2015 which aimed to create ‘islands of TB elimination’? See the six recommendations by Amyn Malik et al.
16 August
Editorial. The EVALI outbreak and vaping in the COVID-19 era. The Lancet Respiratory Medicine 2020, published 14 August. Full-text: https://doi.org/10.1016/S2213-2600(20)30360-X
From August 2019 to February 2020, 2,807 cases of EVALI (e-cigarette, or vaping, product use-associated lung injury) were reported to the CDC, including 68 deaths. Symptoms of EVALI may overlap with those of some infectious respiratory diseases, including COVID-19. This editorial highlights current knowledge and how the effects of vaping might now be colliding with the risk of COVID-19. Several experts have asked for e-cigarettes to be withdrawn from the market during the pandemic.
Bayram H, Köktürk N, Elbek O, et al. Interference in scientific research on COVID-19 in Turkey. Lancet 2020, 396: 463-464, August 15, 2020. Full-text: https://doi.org/10.1016/S0140-6736(20)31691-3
Ethics as a second step? The Turkish Ministry of Health has announced a mandatory application for permission for research on COVID-19, before any application is made to ethics committees. Hasan Bayram and colleagues are worried about these restrictions on independent research in Turkey and hope that the decision will be taken back in compliance with the Turkish Constitution.
14 August
McGuckin B. Dental Triaging: past, present and future. BDJ In Pract 2020;33: 22–23. Full-text: https://doi.org/10.1038/s41404-020-0472-y
Does a ‘lost’ upper anterior crown constitute a dental emergency and require an urgent non-scheduled appointment? It used to be, but in COVID times, it isn’t anymore, despite the emotional distress for the patient. Read these and other considerations in a short overview of dental triage yesterday, today and tomorrow. The next time you go to the dentist, you’ll remember Bronagh McGuckin.
10 August
Nicolay N, Mirinaviciute G, Mollet T, et al. Epidemiology of measles during the COVID-19 pandemic, a description of the surveillance data, 29 EU/EEA countries and the United Kingdom, January to May 2020. Eurosurveillance August 6, 2020. Volume 25, Issue 31. Full-text: https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.31.2001390
Interesting: The number of measles cases declined in the EU and UK in 2020. Reported cases to The European CDC decreased from 710 to 54 between January and May. However, according to the authors, under-diagnoses and under-reporting during the COVID-19 pandemic should be ruled out before concluding that reduced measles circulation is due to social distancing and any community control measures taken to control COVID-19.
9 August
Gluckman TJ, Wilson MA, Chiu S, et al. Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic. JAMA Cardiol 2020, published 7 August. Full-text: https://doi.org/10.1001/jamacardio.2020.3629
Out of fear of contracting SARS-CoV-2, large numbers of patients avoided hospitalization during the COVID-19 pandemic. After analyzing 15,244 hospitalizations involving 14,724 patients with acute myocardial infarction, Tyler Gluckman and colleagues found that patients hospitalized for acute myocardial infarction during the early COVID-19 period had an increased observed/expected mortality ratio which was associated disproportionately with patients with ST-segment elevation myocardial infarction (STEMI).
6 August
Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the Number of US Patients with Newly Identified Cancer Before and During the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Netw Open 2020;3(8):e2017267. Full-text: https://doi.org/10.1001/jamanetworkopen.2020.17267
During and after lockdowns, people go into hibernation mode, but cancer does not. Now Harwey Kaufman and colleagues report a cross-sectional study about patients across the United States who received clinical laboratory testing related to any of 6 cancer types (i.e., breast, colorectal, lung, pancreatic, gastric, and esophageal). Each patient was counted once, at the first instance of a cancer-related ICD-10 code. The authors compared 258,598 patients from the baseline period (January 6, 2019, to February 29, 2020) with 20,180 patients from the COVID-19 period (March 1 to April 18, 2020). During the pandemic, the weekly number of newly identified patients fell 46.4% (from 4310 to 2310) for the 6 cancers combined, with significant declines in all cancer types, ranging from 24.7% for pancreatic cancer (from 271 to 204; p = 0.01) to 51.8% for breast cancer (from 2208 to 1064; p < 0.001). The authors anticipate that a delay in diagnosis will likely lead to presentation at more advanced stages and poorer clinical outcomes.
Matsuo T, Kobayashi D, Taki F, et al. Prevalence of Health Care Worker Burnout During the Coronavirus Disease 2019 (COVID-19) Pandemic in Japan. JAMA Netw Open 2020; 3(8):e2017271. Full-text: https://doi.org/10.1001/jamanetworkopen.2020.17271
How prevalent is burnout among frontline health care workers (HCWs) during the COVID-19 pandemic? Takahiro Matsuo and colleagues conducted an online cross-sectional survey among HCWs at a tertiary hospital in Tokyo which had among the highest numbers of patients with COVID-19 in Japan. Among the final sample of 312 HCW’s, the burnout prevalence was 31.4% (98 of 312). Nurses: 59/126 (46.8%); radiological technologists: 8/22 (36.4%); pharmacists: 7/19 (36.8%). Find more details (i.e., burnout was more prevalent in participants with fewer years of experience) in the paper.
3 August
Mekaoui N, Razine R, Bassat Q, et al. The Effect of COVID-19 on Paediatric Emergencies and Admissions in Morocco: Cannot See the Forest for the Trees? J Trop Pediatr 2020, published 1 August. Full-text: https://doi.org/10.1093/tropej/fmaa046
Where are the sick Moroccan children normally brought to the emergency department? When Nour Mekaoui and colleagues from the Rabat Children’s Hospital, Morocco, compared the number of pediatric consultations (< 16 years) in the emergency department from 16 March to 15 April 2020 with the number of consultations of the same period in the preceding year, they discovered that the number of overall consultations decreased by 74% between the two periods (4232 vs. 1110; p < 0.005). Even the the number of hospitalizations declined (811 in 2019 vs. 471 in 2020, a 41.9% reduction, p < 0.005; see figure). The authors are worried: Where did these severely ill patients go? Might we anticipate a new wave of serious non-COVID-19 pediatric admissions?
23 July
Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral Effect of Covid-19 on Stroke Evaluation in the United States. N Engl J Med 2020; 383:400-401. Full-text: https://doi.org/10.1056/NEJMc2014816
Any decrease in care for patients with ischemic stroke may be consequential because timely treatment may decrease the incidence of disability. The authors compare the mean daily counts per hospital of patients in the pre-pandemic 29-day epoch from February 1, 2020, through February 29, 2020, with the mean daily counts per hospital of patients in a 14-day period during the early pandemic, from March 26, 2020, through April 8, 2020. They found a decrease of approximately 39% in the numbers of patients who received evaluations for acute stroke between two recent periods in U.S. hospitals. The decrease in the use of stroke imaging from the pre-pandemic epoch to the early-pandemic period was seen across all ages, sexes, and stroke severity subgroups.
21 July
Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncology, published: July 20, 2020. Full-text: https://doi.org/10.1016/S1470-2045(20)30388-0
During the UK COVID lockdown, cancer screening was suspended, routine diagnostic work deferred, and only urgent symptomatic cases were prioritized for diagnostic intervention. The authors estimate the impact of diagnostic delays over a 12-month period from the commencement of physical distancing measures, on March 16, 2020, up to 1, 3, and 5 years after diagnosis. They expect an increase in the number of avoidable cancer as a result of the COVID-19 pandemic:
Breast cancer: 281–344 additional deaths (increase: 7.9–9.6%)
Colorectal cancer: 1445–1563 additional deaths (15.3–16.6%)
Lung cancer: 1235–1372 additional deaths (4.8–5.3%)
Esophageal cancer: 330–342 additional deaths (5.8–6.0%)
See also the comment by Hamilton W: Cancer diagnostic delay in the COVID-19 era: what happens next? Lancet Oncology, published: July 20, 2020. Full-text: https://doi.org/10.1016/S1470-2045(20)30391-0
Kamrath C, Mönkemöller K, Biester T, et al. Ketoacidosis in Children and Adolescents With Newly Diagnosed Type 1 Diabetes During the COVID-19 Pandemic in Germany. JAMA. Published online July 20, 2020. Full-text: https://doi.org/10.1001/jama.2020.13445
The COVID pandemic has caused people to delay medical care, even for life-threatening conditions. The authors analyzed data of 532 children and adolescents with newly diagnosed type 1 diabetes from 216 German diabetes centers (median age: 9.9 years). Diabetic ketoacidosis was present in 238 patients (44.7%) and severe ketoacidosis in 103 patients (19.4%). During the same periods in 2019 and 2018, the frequency of diabetic ketoacidosis was significantly lower (2019: 24.5%; 2018: 24.1%). The incidence of severe diabetic ketoacidosis was also significantly lower (2019: 13.9%; 2018: 12.3% in 2018). Children younger than 6 years had the highest risk.
