Copy-editor: Rob Camp
Prevention
Madas BG, Füri P, Farkas Á, et al. Deposition distribution of the new coronavirus (SARS-CoV-2) in the human airways upon exposure to cough-generated droplets and aerosol particles. Sci Rep 2020, published 31 December. Full-text: https://doi.org/10.1038/s41598-020-79985-6
Severe, potentially fatal pneumonia supposes that SARS-CoV-2 reaches the acinar airways. What if we reduced the number of viruses getting there? After characterizing the deposition distribution of SARS-CoV-2 in the airways upon exposure to cough-generated droplets and aerosol particles, Balázs Madas et al. found that the number of viruses deposited in the extra-thoracic airways is about 7 times higher than in the acinar airways. The authors hypothesize that most cases of COVID-19 pneumonia might be preceded by SARS-CoV-2 infection of the upper airways and that without the enhancement of viral load in the upper airways, COVID-19 would be much less dangerous. Ergo, we should use the period between the onset of initial symptoms and the potential clinical deterioration to block or significantly reduce the transport of virus towards the acinar airways, for example with non-specific treatment forms like disinfection of the throat and nasal and oral mucosa. In any case, recommend the authors, use a tissue or cloth in order to absorb droplets and aerosol particles emitted by your own coughs and sneezes… before re-inhalation! Even if you are alone in quarantine.
Vaccines
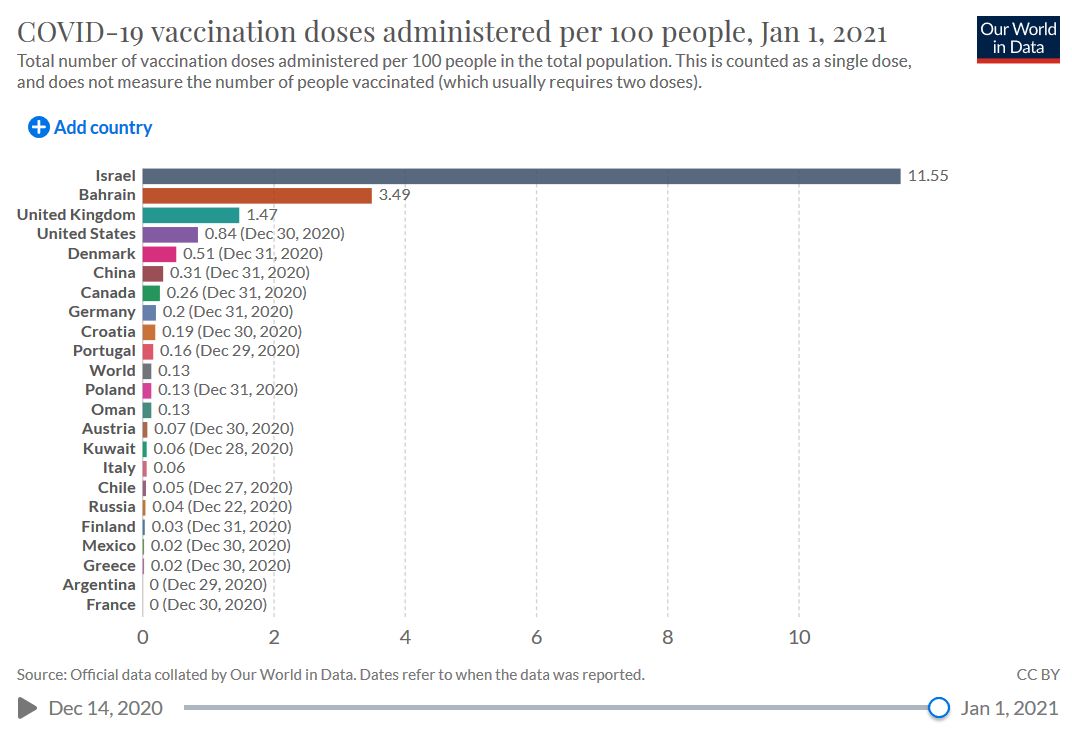
Kershner I. How Israel Became a World Leader in Vaccinating Against Covid-19. The New York Times 2021, published 1 January. Full-text: https://www.nytimes.com/2021/01/01/world/middleeast/israel-coronavirus-vaccines.html
Badly hit by the coronavirus, Israel has distributed the first of two vaccine doses to more than 10 percent of its population.
Clinical
Shapiro J, McDonald TB. Supporting Clinicians during Covid-19 and Beyond — Learning from Past Failures and Envisioning New Strategies. N Engl J Med 2020, published 31 December. Full-text: https://doi.org/10.1056/NEJMp2024834
Clinicians are facing important emotional stressors during the COVID-19 pandemic, including grief from seeing so many patients die, fears of contracting the virus and infecting their family members, and anger over health care disparities and other systems failures. Jo Shapiro and Timothy McDonald show the way medical institutions should follow to design emotional-support programs that clinicians will embrace. The last of four suggestions: institutional leadership should be accountable for clinicians’ well-being. Leaders should empower clinicians to speak up about unsafe, highly stressful or morally challenging workplace conditions and ensure that concerns are listened to and, whenever possible, acted on.
Severe COVID
Maximous S, Brotherton BJ, Achilleos A, et al. Pragmatic Recommendations for the Management of COVID-19 Patients with Shock in Low- and Middle-Income Countries. Am J Trop Med Hyg. 2020 Dec 21. PubMed: https://pubmed.gov/33350378. Full-text: https://doi.org/10.4269/ajtmh.20-1105
The authors suggest using Sequential Organ Failure Assessment (qSOFA) and point-of-care ultrasound (POCUS) for evaluation purposes to use fluid therapy, norepinephrine and low-dose corticosteroids depending on etiology. The authors also recommend avoiding the routine use of central venous or arterial catheters and using simple bedside measures such as capillary refill time to address targets of resuscitation.
Comorbidities
Fernandez-Ruiz R, Paredes J, Niewold TB. COVID-19 in patients with Systemic Lupus Erythematosus: Lessons learned from the inflammatory disease. Transl Res. 2020 Dec 19:S1931-5244(20)30302-9. PubMed: https://pubmed.gov/33352298. Full-text: https://doi.org/10.1016/j.trsl.2020.12.007
The authors review the literature to date on COVID-19 in patients with systemic lupus erythematosus (SLE) and provide an in-depth review of current research in the area, including immune pathway activation, epidemiology, clinical features, outcomes, and the psychosocial impact of the pandemic in patients with SLE.
Collateral Effects
Van Haren RM, Delman AM, Turner KM, et al. Impact of the COVID-19 Pandemic on Lung Cancer Screening Program and Subsequent Lung Cancer. J Am Coll Surg. 2020 Dec 12:S1072-7515(20)32525-4. PubMed: https://pubmed.gov/33346080. Full-text: https://doi.org/10.1016/j.jamcollsurg.2020.12.002
Low-dose computed tomography (LDCT) screening reduces lung cancer mortality by at least 20%. At the University of Cincinnati, COVID-19 caused significant disruption in lung cancer screening, leading to a decrease in new patients screened and an increased proportion of nodules suspicious for malignancy once screening resumed.
Education
Rubin EJ, Baden LR, Barocas JA, Morrissey S. A Look at Covid-19 Prevention and Care in 2020. Audio interview (26:46). N Engl J Med 2020; 383: e147. Access: https://doi.org/10.1056/NEJMe2036225
The editors discuss the new mRNA-1273 vaccine against SARS-CoV-2, along with other studies of native and exogenous antibodies.
Copy-editor: Rob Camp
